Cancer Survivorship
Cancer survivorship involves understanding the complexities of cancer survivorship and providing the necessary support. It refers to the stage of a person’s life after being diagnosed and treated for cancer. It is not only about post-cancer life but also includes a holistic approach to a person’s health, well-being and quality of life after completion of treatment. Survival is not only about physical fitness but social psychological, emotional as well as social factors. Survivor care focuses on managing the continuum of health. Dealing with the long-term delays of cancer treatment, and supporting the individual through the transition from treatment to life after cancer.
By the end of this section, you should know:
- The concept of cancer survivorship.
- The influence of cancer survivorship on patients’ quality of life.
- The effects that cancer has on the family.
- The nursing implications related to cancer survivorship.
- The essential components of survivorship care.
Let’s take a closer look at them.
Test Your Knowledge
At the end of this section, take a fast and free pop quiz to see how much you know about Cancer Survivorship.
The Concept of Cancer Survivorship.
Cancer survivors are defined as individuals living with, though, or beyond cancer. And survivor care includes addressing their unique medical, psychosocial, and social needs. A survivor’s journey can take years, and the model of care includes long-term follow-up, prevention, health promotion, and lifestyle changes.
Cancer Survivorship: The phase of a person’s life following the diagnosis and treatment of cancer. It involves the ongoing care, monitoring, and management of physical, emotional, and social issues that arise post-treatment. Survivorship care includes addressing late or long-term effects of cancer treatment and providing support for health and well-being.
The Influence of Cancer Survivorship on Patients’ Quality of Life.
Cancer survival significantly affects patients’ quality of life (QOL) in a variety of ways, both positively and negatively.
Physical effects: Survivors often experience long-term side effects from treatment, including fatigue, pain, neuropathy, psychosis, and fertility issues. These side effects may persist long after treatment is completed, thus requiring continued monitoring and management.
Psychosocial consequences: Survivors often experience psychological complications such as anxiety, depression, and posttraumatic stress disorder. The emotional toll of cancer can affect relationships, work, and mental health in general. Many survivors experience isolation or a sense of loss. Especially when it comes to changes in their bodies, lifestyles, or future plans.
Social impact: Cancer survivors may also face challenges in returning to life after treatment. They may feel disconnected from peers who do not understand their experience. Or find it difficult to return to work or manage family dynamics after cancer.
Despite these challenges, some survivors are more resilient, have a greater appreciation for life, and a stronger sense of purpose. With appropriate care, psychological support, and rehabilitation services, quality of life can be improved.
Neuropathy: A condition that results from damage to the nerves, leading to symptoms like pain, numbness, tingling, or weakness. Neuropathy can be caused by cancer treatments such as chemotherapy (chemotherapy-induced peripheral neuropathy) or by the cancer itself.
The Effects that Cancer has on the Family.
Cancer affects not only the individual diagnosed but also their family members, who experience significant distress and disruption in their daily lives. The impact varies depending on the family structure. which may include nuclear families, extended families, single-parent families, close friends, or blended families. Despite being a 2006 study, the summary of issues affecting families of cancer patients remains highly relevant today (Lewis, 2006).
Key Issues Faced by Families of Cancer Patients:
- Distress Among Family Members: When a family member is diagnosed with cancer, the entire family is affected. The distress experienced by loved ones may be emotional, psychological, and physical, as they navigate the changes in their family dynamics due to the illness.
- Lack of Understanding and Support: Family members often struggle to understand and respond supportively to each other’s emotional expressions and behaviors related to the cancer diagnosis. This lack of mutual understanding can create tension, misunderstanding, and stress within the family unit.
- Coping with Cancer’s Impact: Families attempt to manage the impact of cancer while dealing with internal tensions and strains exacerbated by the disease. This includes balancing the needs of the patient with the emotional and practical needs of other family members.
- Challenges for Long-Term Survivors: When a family member becomes a long-term cancer survivor, the family faces the challenge of maintaining normalcy. Survivors may require ongoing medical attention, while family members may feel uncertain about how to provide appropriate support or deal with lingering health effects.
Family Caregiving: A Stressful Experience towards Cancer survivorship
Caregiving responsibilities often fall on a family member, who becomes the primary support for the patient. This can be a demanding and stressful experience, influenced by several factors:
Caregiver Role and Relationship: The emotional burden and difficulty of caregiving can vary depending on the closeness of the relationship between the caregiver and the cancer patient, as well as the progression and severity of the disease.
The “Sandwich Generation”: Family caregivers, particularly those between the ages of 30 to 50, face the challenge of caring for both their own children and elderly parents with cancer. This generation often juggles the emotional, physical, and financial demands of both family and caregiving responsibilities.
Demands of Family Caregiving
Physical Demands: Caregivers assist with day-to-day activities such as bathing, feeding, toileting, or dressing, especially in advanced stages of cancer.
Psychological and Emotional Demands: Caregivers must navigate complex emotional needs, including offering emotional support, helping with decision-making, and solving problems related to the patient’s condition.
Social and Economic Demands: Family members must balance caregiving with social obligations and work commitments. Financial strain often arises, especially if a caregiver needs to reduce work hours or stop working altogether to provide care.
Impact of Cancer Survivorship on Family Function
When one family member is living with cancer, the entire family often faces disruption in their usual roles and functions. Some of the core family functions affected include:
Creating a Safe and Supportive Environment: The family must maintain an emotionally and physically safe space, both for the cancer patient and the other family members, while dealing with the stresses associated with the illness.
Managing Stress: Cancer and its treatment often induce stress, and families must find ways to interpret, reduce, and manage the stressors they face.
Parenting and Child Care: In families with children, the challenge of maintaining a nurturing and supportive environment for children is crucial. Children may need to be informed about the illness and supported emotionally as they cope with their changing circumstances.
Uncertainty About Roles: Spouses and other family members often face uncertainty about their roles in providing support. They may feel unsure about how to help, and roles within the family can become fragmented as everyone adjusts to the patient’s needs.
The Nursing Implications Related to Cancer Survivorship.
Nurses play an important role in the care of cancer survivors, advocating for and supporting the physical, emotional and psychological well-being of cancer survivors
Assessment and monitoring: Nurses should frequently assess for physical symptoms such as fatigue, pain, myalgia, or other long-term or delayed effects of treatment. Symptoms of psychological distress such as anxiety, depression, or PTSD should also be assessed and patients referred to mental health professionals when necessary.
Education and support: Nurses are responsible for providing education about the risks of cancer recurrence, preventing secondary cancer, making appropriate lifestyle changes (such as diet, exercise- exercise, and smoking cessation), and deal with long-term consequences. Providing emotional support and helping survivors cope with the challenges of life after cancer is an important part of nursing care.
More Implications
Coordination of care: Nurses act as intermediaries between specialist, primary care and oncology teams to ensure care is well coordinated and comprehensive. Survival care generally requires a team approach to meet a patient’s needs.
Advocacy: Nurses recommend the development and implementation of survivor care plans, ensuring that survivors receive needed follow-up care, testing, and ongoing resource development. They can help survivors understand and manage insurance or financial issues related to continuing care.
Psychosocial support: Nurses need to be sensitive to the psychological and emotional impact of having cancer. Providing a safe space for patients to express their concerns and connecting them with social services or support groups can help prevent mental illness.
Oncology: The branch of medicine focused on the study, diagnosis, treatment, and management of cancer. Oncologists are specialists who care for individuals with cancer, using a variety of treatments like surgery, chemotherapy, radiation therapy, and more.
Post-Traumatic Stress Disorder (PTSD): A mental health condition triggered by experiencing or witnessing a traumatic event, such as a serious illness like cancer. Individuals with PTSD may experience flashbacks, nightmares, anxiety, depression, and other emotional responses. Cancer survivors may develop PTSD related to their diagnosis and treatment.
Radiation Therapy: A treatment that uses high-energy radiation to kill or damage cancer cells. It is often used to shrink tumors before surgery, eliminate remaining cancer cells after surgery, or alleviate symptoms caused by cancer. Radiation therapy can be external (delivered from outside the body) or internal (delivered via radioactive materials placed inside the body).
The Essential Components of Cancer Survivorship Care.
The Institute of Medicine (IOM) describes four basic components of survivorship care that are necessary to support cancer survivors:
Prevention and detection of new cancers and cancer recurrences
Survival care includes ongoing care for new cancers or recurrence of the original cancer. This often requires regular checkups, tests and tests to detect the first signs of cancer recurrence or secondary recurrence.
Monitoring metastasis, recurrence, or secondary cancer
The surveillance programs are designed to monitor the survivor’s health and check for any signs of cancer spread or recurrence. Care usually includes physical exams, imaging, and laboratory tests as recommended by oncologists.
Interventions for cancer outcomes and treatment
Many cancer survivors experience long-term side effects from their treatments, including fatigue, pain, mood changes and hormonal imbalances. Survivorship care should address these symptoms with appropriate interventions such as medication, physical therapy, counseling, and lifestyle changes
Communication between specialists and primary care providers
Caring for a survivor requires a team approach. Oncologists, primary care providers, specialists (e.g., cardiologists, endocrinologists), psychiatrists, and dieticians must work together to ensure continuity of care Coordination of care between different providers ensures that all aspects of survivor health have been addressed.
Other measures often include psychological support, addressing sexual health and reproductive problems, and providing educational materials for healthy living It is important to have a well-developed survival care plan to ensure that these items are met.
Cancer Survivorship Care Plan (SCP)
To meet the complex needs of cancer survivors, the Survivorship Care Plan (SCP) is vital. This care plan, developed by the patient’s oncology provider, includes a comprehensive overview of the treatment history and detailed instructions for follow-up care, future screening, and managing potential long-term effects. The SCP typically includes:
Care Summary:
Diagnostic test results, tumor characteristics, and details of treatments provided (e.g., surgery, chemotherapy, radiation).
Contact information for healthcare providers involved in the patient’s care.
Identification of a care coordinator who oversees the survivor’s care.
Follow-Up Plan:
Recommendations for cancer screenings and tests.
Information on late or long-term effects of cancer treatments.
Guidelines for maintaining healthy behaviors (e.g., exercise, nutrition, avoiding smoking).
Referrals for genetic counseling, if appropriate, and resources for support.
Example Scenario: Mrs. Henry
In an example scenario, Mrs. Henry, a 45-year-old breast cancer survivor, comes for her first physical examination after treatment. When asked to bring her survivorship care plan, she reveals that she doesn’t have one. The nurse’s best response would be to:
Acknowledge the importance of having an SCP and explain the need for the patient’s primary care provider to coordinate her post-treatment care.
Assure her that even though she may not have received one, the primary provider can create or refer her to a survivorship care plan, which will be crucial for her ongoing health management.
Assess her health status, paying special attention to any late effects of treatment (e.g., fatigue, neuropathy, or psychological symptoms) and perform relevant physical and psychological assessments.
This approach ensures that the patient’s needs are addressed in a holistic manner, and supports ongoing care that is well-coordinated between oncology specialists and primary care providers.
Barriers and Challenges in SCP Development
Several challenges hinder the development and implementation of Survivorship Care Plans (SCPs):
- Financial and Human Resource Constraints: The costs of creating an SCP and the lack of reimbursement. These services make it difficult for healthcare providers to prioritize them. For instance, insurance may not cover the development costs, and reimbursement for related assessments is often low (e.g., 38% from private insurance, 59% from Medicare/Medicaid).
- Lack of Universal Standards: Not all cancer centers, particularly non-NCI-designated centers, provide SCPs, leaving many survivors without a clear post-treatment care plan.
- Inequities in Access: Many survivors do not have access to comprehensive care centers and may not receive the necessary guidance or referrals to manage their health following treatment.
The Role of Nurses in Cancer Survivorship Care
Nurses play a critical role in bridging these gaps by recognizing cancer survivors and ensuring they are connected with the necessary resources. They can advocate for the development of Survivorship Care Plans, educate patients on the potential long-term effects of cancer treatment. And work closely with interprofessional teams to ensure that both cancer-related and non-cancer-related health issues are addressed. By working collaboratively, nurses and other healthcare providers can offer survivors a well-rounded approach to care. Ensuring both treatment-related problems and future health risks are managed effectively.
A cancer diagnosis poses many challenges and responsibilities for nurses, especially in managing long-term health outcomes and helping patients and their families adjust to life after cancer. Nurses are well positioned to play an important role in improving public health strategies for survivorship care. as well as educating patients and healthcare professionals about the realities of cancer survivorship. Here we explore key ways in which cancer survival is integrated into nursing practice
Social Research
Cancer survivors are important members of the health care system, and it is important for nurses to consider the unique needs of these patients. An important step in this process is gathering detailed information from survivors, as this enables nurses to understand their experience and tailor care accordingly by asking open-ended questions such as “How was your cancer diagnosis and treatment?” during nursing history. or “How does your situation affect you now?” Such questions help to generate detailed, contextual information that provides valuable insight into the survivor’s journey.
Highlights of Survival Analysis
Known cancer history: Some patients do not immediately disclose their cancer history, so direct questions about prior surgery, chemotherapy, radiation, or hormone therapy are necessary to elicit information which is appropriate.
Understanding the long-term effects of cancer treatment: Nurses need to recognize the specific short- and long-term effects of cancer treatment and assess how it affects the patient’s current health and coexisting conditions such as heart disease.
Symptom Management: Many cancer survivors continue to face symptoms related to their cancer or its treatments. Nurses should explore symptoms like pain, fatigue, neuropathy, and cognitive changes, asking targeted questions like, “Since your cancer treatments, have you noticed any changes in your memory or ability to concentrate?”
Genetic Counseling and Risk Assessment: Following new standards from the American College of Surgeons Commission on Cancer, all accredited centers must incorporate genetic counseling and risk assessment into patient care. Nurses play a critical role in identifying survivors who may benefit from these services.
Symptom Management
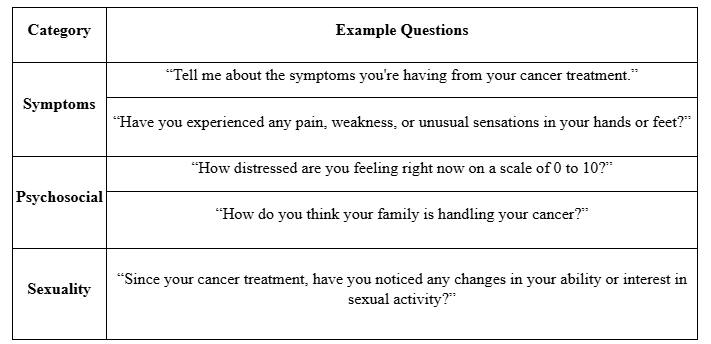
For cancer survivors, symptom management remains an ongoing challenge. Nurses must assess and address symptoms that continue post-treatment, such as chronic pain, neuropathy, fatigue, and psychological distress. It’s important to not only identify the symptoms but also explore their impact on the survivor’s quality of life (QOL).
Examples of Assessment Questions for Cancer Survivors:
Patient Education
Patient education is critical to empowering cancer survivors to manage health care post-treatment. Nurses should assess whether a patient is primarily self-care or needs assistance from a caregiver. Effective education must be tailored to the needs of the individual, to help manage their ongoing health challenges and self-care behaviors.
Transactional model of cancer family care: Nurses should use models such as Schumacher et al.’s transactional model of cancer family caregiving to understand the relationship between patients and caregivers. This model illustrates three models of care: self-care, shared care, and family care. It will guide educational efforts to understand where the patient and caregiver are on this continuum.
Self-care and symptom management: It is important for cancer survivors to learn how to manage chronic symptoms such as muscle pain or fatigue. For example, if arthritis is present, patients should be taught how to protect the foot, prevent falls, and manage thermal sensations.
Health promotion and lifestyle behaviors: Nurses should guide survivors in adopting appropriate lifestyle behaviors to improve their long-term health. This includes encouraging exercise, a healthy diet, smoking cessation and regular screening to detect secondary cancers or chronic conditions.
Providing Resources
Nurses need to be proactive in referring people with cancer to appropriate facilities. While there are many community-based survivor support organizations, the information is often inconsistent. Nurses need to be familiar with available resources and ensure that patients are connected to the appropriate services they need.
Cancer support organizations: Organizations such as the American Cancer Society (ACS) and the National Coalition for Cancer Survivorship (NCCS) provide many free services, such as counseling, financial assistance, and educational materials.
Clinical resources: Nurses need to be knowledgeable about resources in their health care system, such as clinical support services, NCI-designated cancer centers, and clinical trials that can provide patients with cutting-edge treatments.
Community services: Many cancer survivors require assistance with transportation, child care, home care, and financial support. Nurses should help survivors navigate these needs by connecting them with local resources and community services.
Chemotherapy: A treatment for cancer that uses drugs to destroy cancer cells or inhibit their growth. Chemotherapy works by interfering with the cancer cell’s ability to divide and multiply but can also affect healthy cells, leading to side effects.
Hormone Therapy: A treatment used in certain cancers that are sensitive to hormones, such as breast and prostate cancer. It works by either blocking the body’s ability to produce hormones or by interfering with how hormones affect cancer cells. This therapy can involve medications or surgical procedures to reduce hormone levels.
