Community-Based Nursing
This section explores the vital connection between public health and community health nursing, focusing on the roles of nurses in community-based practice and their care for vulnerable populations. You will also learn about key competencies, the elements of a community assessment, and strategies for improving health outcomes. Let’s dive in!
By the end of this section, you should be able to know about the:
- Relationship between public health and community health nursing.
- Community health nursing from community-based nursing.
- Role of the community health nurse.
- Role of the nurse in community-based practice.
- Characteristics of patients from vulnerable populations that influence the community-based nurse’s approach to care.
- The competencies important for success in community-based nursing practice.
- Elements of a community assessment.
Let’s take a closer look at them.
Test Your Knowledge
At the end of this section, take a fast and free pop quiz to see how much you know about Community-Based Nursing Practice
Relationship between public health and Community-Based Nursing
People use Community-Based Nursing and public health nursing terms interchangeably, but they have distinct areas of focus. Public health nursing emphasizes understanding the needs of populations or groups with similar characteristics, such as high-risk infants or older adults These nurses focus on health promotion, maintenance, and systemic change to enhance public health. Their work often involves screening for various diseases, analyzing the environment and recommending programs such as safer playground equipment. Public health nursing generally requires a bachelor’s degree in nursing, and possibly as part of a major.
In other words, Community-Based Nursing focuses on providing care directly to individuals, families, and groups in the community to improve overall health outcomes. This practice addresses the needs of specific subpopulations, such as older adults who require rehabilitation or vaccination to prevent infectious diseases. Educational requirements about community health nursing are less relevant than public health nursing, and they do not require advanced degrees.
Achieving progress in community health care requires physicians to possess broad social and political skills, including the capacity to exercise power designed for community development. While entry requirements may not be rigorous, effective practice requires strong public health principles, family theory, and communication skills. Community health nurses often work in social settings in difficult circumstances and face challenges such as opposition to welfare programs. Strong advocacy and business skills are essential in navigating these developments.
More about the public health and Community-Based Nursing
Community health nursing includes specialized skills. Nurses conduct population-focused research, assessing community needs by assessing individual and family health concerns. Critical thinking is essential, as nurses use public health knowledge, community health considerations, and an understanding of family dynamics to design effective interventions. Building strong relationships with community members and leaders is also key. For example, if there is a tendency for grandparents to take on more of a caregiving role, the Community-Based Nursing nurse can develop a supportive program in collaboration with local schools.
An example of Community-Based Nursing practice could involve identifying trends like grandparents taking on childcare responsibilities. In response, nurses might create educational initiatives, collaborate with community leaders, and leverage local resources to establish supportive programs. Their role often includes advocating for resources and working within resistant systems to implement effective health initiatives that address community-specific needs.
Community Health Nursing: Community-Based Nursing involves a broader approach to healthcare that focuses on the health needs of entire communities or specific populations. This practice combines elements of public health and nursing to assess community health, advocate for public health policies, and implement health promotion and disease prevention strategies.
Public Health Nursing: Public health nursing is a specialized nursing practice focused on improving the health and well-being of populations through community assessment, policy advocacy, and preventive health services. Public health nurses work to identify and address health issues affecting entire communities and promote equitable access to healthcare resources.
Community health nursing from community-based nursing and the Role of the community health nurse
Everyone knows that Community-based care prioritizes health promotion, disease prevention, and restorative care. This is by delivering healthcare services directly where people live, work, socialize, and learn. The community-based healthcare model ensures collaboration and practices that are based on evidence to address community health needs. There are some essential elements of a healthy community including safety, healthcare access, and factors that foster productivity. Additionally, nurses play a strategic role in community-based care by improving community health and focusing on holistic, preventative care practices.
Key Components of Community-Based Nursing Health Care
All members of the community are being targeted by the Community-based healthcare including underserved groups. It assures the primary care and health promotion outside of the traditional healthcare facilities such as hospitals. Moreover, services cover both acute and chronic conditions, delivered directly within communities.
Challenges in Community-Based Nursing Health Care
There are several challenges that face Community-based healthcare. And they are influenced by Political policies such as the Affordable Care Act, social determinants of health such as socioeconomic factors, education, health disparities between different groups, and economic factors that are impacting healthcare accessibility.
Common public health issues include many things such as the lack of adequate health insurance, the chronic illnesses (e.g., heart disease, diabetes), the under-immunization in children, and the STI increases.
Achieving Healthy Populations and Communities
Improving the health status of the Americans through setting healthcare goals is aimed by The Healthy People Initiative by the USDHHS. Healthy People 2020 targets increasing life expectancy, the quality of life, and reducing health disparities.
Improving Healthcare Delivery
Improved healthcare delivery relies on:
- Assessment like collecting data on population health, monitoring health statuses, and accessing community health information.
- Policy Development such as creating policies based on community assessments, such as lead cleanup programs for communities with high lead poisoning levels.
- Access to Care like ensuring community health services are available and accessible to all members.
Evidence-Based Practice in Community Settings
Improving the outcomes for specific health needs in community settings are being done by Evidence-based practices. This is exemplified by prostate cancer screening (PCS) in community centers. Moreover, these centers that provide culturally appropriate information and decision-making support encourage better health outcomes, especially for underserved groups. Key strategies include:
- The increase of patient knowledge on screenings,
- Reinforcing decision-making rights,
- Community social and cultural dynamics understanding,
- The involvement of family in educational sessions when appropriate.
Social Determinants of Health
There are a lot of factors that influences the health such as social determinants of health:
- Biology and genetics like age, sex,
- Individual behavior such as substance use, sexual practices,
- Social environment like income, discrimination,
- Physical environment like the living conditions, and
- Health services as the access to quality care.
Health Disparities
Health disparities here refer to preventable differences in health burdens or opportunities. Those also affect the populations based on factors such as race, gender, socioeconomic status, or geographic location. Additionally, they are typically related to historical and current inequalities in social, political, economic, and environmental resources. It is known that the reduction of these disparities may require addressing various factors, like poverty, inadequate healthcare access, and educational inequalities.
Community-Based Nursing: Community-based nursing focuses on providing care to individuals and families in a specific community setting, such as in their homes, schools, or local clinics. This type of nursing emphasizes direct care for acute and chronic conditions, continuity of care, and coordination of local resources to meet the unique health needs of individuals and families.
Health Disparities: Health disparities are differences in health outcomes and access to healthcare services that exist between different population groups. These disparities are often influenced by factors such as socioeconomic status, race, ethnicity, geographic location, and access to quality healthcare.
Population: In public and community health, a population is a specific group of people, often defined by geographic, demographic, or health-related characteristics, who share common health needs or risks. Populations can be as large as entire communities or as specific as vulnerable groups with particular health challenges.
Social Determinants of Health: Social determinants of health are the non-medical factors that influence health outcomes, including conditions in which people live, work, and socialize. Examples include income, education, employment, social support networks, and access to healthcare. These determinants play a significant role in shaping health disparities.
Role of the nurse in Community-Based Nursing practice
Nurses play an important role in improving patient health in community practice. Additionally, nurses interact with a variety of people in a variety of settings. They learn to recognize local resources and tailor care to individual patients. There is continuity of care mechanisms that avoid duplication and ensure efficient use of resources. For example, the nurse can coordinate wound care for the patient. And help their family heal at home by providing low-cost supplies.
Special strategies for health promotion in the community
Evidence-based strategies are needed to improve patient outcomes in the community. Research shows the value of such approaches, such as interventions that address certain health issues. To improve health outcomes, for example, community nurses used focused strategies. Those to help patients with chronic obstructive pulmonary disease (COPD) manage themselves, prevent panic attacks, and follow medication protocols (Kirkpatrick et al., 2012). Similarly, culturally sensitive assessments have been included to help men of specific ethnic groups make informed decisions about prostate cancer screening. Assuring that treatment is appropriate for their cultural needs and values (Chan et al., 2011 Gash & McIntosh, 2013). This is referred to as evidence-based interventions.
The second is establishing strong relationships. Close relationships with patients and their families are essential to exploring the big picture of each patient’s life. This relationship is the basis for providing insightful advice, instruction and guidance. Here are some variables: family dynamics, policies, child care arrangements, and cultural norms are important factors that nurses can change in health care so that patients can continue to lead normal lives. For example, when planning follow-up care, the nurse considers the patient’s needs or the availability of a family member to care for the children
Adjusting for family and community variables is also an important strategy. It is recommended that nurses focus on broader factors such as family values, structures, social norms, and community factors that shape health behaviors and lifestyles in families and communities. This allows nurses to develop community-based programs that promote health, prevent disease, and address unique family and community dynamics.
Key Points in Community-Based Nursing Practice
Public Health Principles: Community-Based Nursing is rooted in principles that promote a healthy living environment, involving community assessments, policy advocacy, and resource access.
Population-Based Effectiveness: Effective population-based health services enhance the overall health of the community by preventing diseases and promoting wellness.
Holistic Care Approach: Community health nurses serve both the community as a whole and individuals, ensuring that each patient is viewed within the larger context of their community.
Adaptability and Responsiveness: Nurses build relationships within communities, adapting to changes and responding to emerging health needs.
Competency in Multiple Roles: Community-based nurses fulfill various roles—caregiver, collaborator, educator, counselor, change agent, patient advocate, case manager, and even epidemiologist—enabling them to address complex and chronic conditions, particularly for vulnerable populations.
Addressing Vulnerable Populations
Caring for vulnerable populations with complex health conditions is a significant challenge. Community-based nurses use their skills to provide comprehensive care that addresses acute and chronic needs. By understanding patients’ social, economic, and health disparities, nurses can better advocate for resources, tailor interventions, and collaborate with community services to ensure these populations receive adequate care and support.
Characteristics of patients from vulnerable populations that influence the community-based nurse’s approach to care.
Care is provided through community-based nurses in settings such as homes or hospitals. Care focuses on individual and family needs to address acute and chronic health problems, ensure safety, promote self-care, and support patient autonomy in decision-making. In order to assess health status to identify problems, plan, implement, Monitoring and evaluation are needed. And, an understanding of community needs and perspectives is important in planning care.
Nursing facilities are the initial point of contact between patients and the health system. Care can be delivered closer to where people live to lower healthcare costs and improve access to care. Additionally, these centers often serve vulnerable populations, including many without access to traditional health care.
Vulnerable populations in Community-Based Nursing
Other risk factors, lack of access to care, and dependence on others had placed vulnerable populations at increased risk for health problems. For example, in addition to poor individuals, the elderly, immigrants, those in abusive relationships, drug addicts, and individuals with serious mental illness, nurses provide important health development, early detection, and prevention for these groups.
Types of Difficulties in Community-Based Nursing:
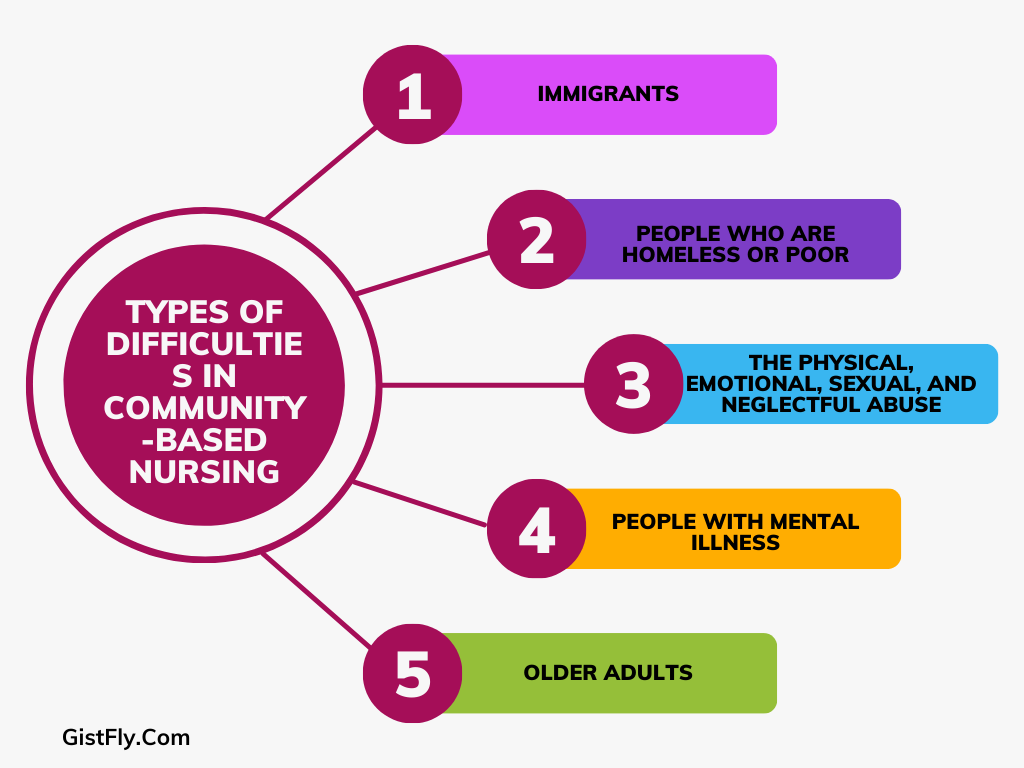
1. Immigrants who typically use unconventional medicine have fewer finances, fewer health problems, and fewer language barriers. Their health may deteriorate and their life expectancy may be shortened because many of them develop asthma.
2. People who are homeless or poor. While homelessness doubles the risk of hardships, including inadequate nutrition and shelter, and severe chronic diseases, poverty is known to exacerbate more pronounced health disparities
3. The physical, emotional, sexual, and neglectful abuse endured by some patients affects all age groups. In addition, nurses are required to protect vulnerable patients, report abuse, and frequently interview patients in private to facilitate open discussions
4. People with mental illness who may face socioeconomic and health challenges, including homelessness and unemployment. Mental health services are community based rather than institutional focused. This requires nurses to support the integration of patients and living in the community.
5. Older adults: The fact that the population is growing means that the demand for healthcare services to manage chronic diseases and improve quality of life is also increasing. In addition, nurses provide this group with health promotion, chronic disease management, and lifestyle guidance.
Guidelines for assessing vulnerable populations
Nurses must provide effective care by:
• To create a non-threatening environment so that patients feel comfortable and understood.
• Use culturally appropriate practices. They know they need to understand that patient’s cultural beliefs, be able to work with the help of an interpreter, and avoid judgments based on their own beliefs.
• By addressing social determinants, this consists of determining whether patients will have immediate non-health care concerns such as financial and legal problems.
Assessment Process
- Nursing History can be done by collecting comprehensive information to check family-centered needs, such as risks to the immune system, and this is especially for homeless patients.
- Physical and Home Assessment that happens after evaluating for signs of abuse, substance issues, and environmental risks in the patient’s home.
Barriers and Health Outcomes for Vulnerable Populations
Vulnerable people usually face big barriers to accessing healthcare. Those barriers are financial limitations and lack of local services. The consequences are poorer health outcomes, shorter lifespans, and higher morbidity rates. Nurses are essential in assessing patients’ strengths, coping abilities, and resources to provide effective, community-based care.
Competency Requirements for Community-Based Nursing Nurses
In order to meet the needs of diverse, vulnerable populations, community-based nurses need to be highly skilled in critical thinking, cultural competence, communication, and community assessment. Also, to help patients through complicated healthcare and social difficulties in a community context, they must modify their approach to each patient’s particular social and cultural background.
Roles of Community-Based Nursing Nurses
There are many roles for the Community-based nurses. Those roles allow them to meet diverse patient and community needs. Now these roles include direct care, health promotion, disease prevention, and helping patients navigate healthcare systems.
Community nurses play diverse and important roles in improving the health of individuals, families, and communities. As caregivers, they manage the health of people in the community by applying nursing practice and critical thinking to self-management. Traditionally focused on pediatric health, community nurses now address broader issues such as homelessness, uninsurance, which expand their pediatric health care. They develop long-term partnerships with patients and families, identify health needs and connect resources to promote health and safer communities.
In their role as case managers, community nurses plan and coordinate care by developing assessment-based individual care plans. They often manage multiple patients, directing continuums of care and collaborating with providers and payers. This requires a deep understanding of the constraints, constraints, and opportunities of a particular community.
As agents of change, nurses work to solve problems by developing new and effective ways to address health challenges in families and communities. They address issues such as access to child care, adult day care, and violence, and empower families to find solutions. Change implementation may involve conflict management, which will require nurses to mediate between providers and clarify roles to better serve patients.
Community nurses act as patient advocates, guiding individuals through the complex health care system by providing information about services, liaising with authorities, and providing follow-up support. They ensure that patients are created to inform decisions to be made and defend these decisions within the system when needed.
Another Role
Another important role for community nurses is collaboration. They work in multidisciplinary teams to develop care plans that align with shared goals, such as cases that require end-of-life care. Successful communication depends on building respect and trust among team members.
As counselors, community nurses help patients identify health problems and choose actions to address them. They provide supportive, non-judgmental guidance and empower patients by helping them identify barriers and solutions, and encourage informed decision-making.
In their educator roles, community nurses educate patients and groups on topics such as prenatal care, child safety, and chronic disease management. They assess learning needs, provide follow-up support, and help patients develop the skills necessary to manage their health. The continuity of Community-Based Nursing allows for ongoing learning, reinforcing good practice.
Finally, as epidemiologists, community nurses monitor and manage health risks in the community. They track issues like infectious diseases, lead exposure, and pregnancy trends, observing changes in health status, identifying causes, and maintaining public health levels through targeted interventions.
Vulnerable Populations: Vulnerable populations are groups that are at increased risk for poor health outcomes due to factors such as socioeconomic status, chronic health conditions, limited access to healthcare, or other social determinants of health. These populations may include the elderly, low-income individuals, minority groups, and people with disabilities, among others.
The competencies important for success in Community-Based Nursing practice And the Elements of a community assessment
To be able to develop successful health interventions and comprehend the context where patients live, community-based nurses must evaluate the larger community. The methodical process of collecting information about the ecology and health of a community is known as community assessment. Nurses can recognize and treat health problems at the individual and community levels with this approach (Stanhope & Lancaster, 2014).
Components of Community Assessment
There are three main components the community assessment focuses on: structure or locale, population, and social system. Each of these elements provides critical insights into the community’s health needs, resources, and potential challenges.
Structure or Locale: this component describes a community’s organizational and physical characteristics. Understanding the geographic borders, the water and sanitation systems, the housing quality, the emergency services, the transportation networks, and the economic circumstances like the average household income and the rates of public assistance are all important components. Moreover, examining the structure of the neighborhood and the ease of access to services aids in evaluating the community’s design, the availability of necessary services, and the locations of social meeting places. Then there is the Population that shows the demographic traits of the community’s residents.
It has also some important components such as the distribution of ages and sexes, population growth patterns, density, educational attainment, the majority of ethnic and religious groupings, and other demographic characteristics. The nurses can predict certain health needs, such as childcare services in communities with a high proportion of young families or geriatric care in places with a greater old population, by analyzing local census data or health department records to determine population demographics. And finally, there is the Social System that consists of the organizations and assets. Those assist the community’s social and medical requirements. Social systems comprise the health system, welfare programs, volunteer organizations. Additionally Social systems comprise Local government, education system, and communication infrastructure .
Gathering Information for Community Assessment
Collecting data through both observation and research community assessments by the nurses requires many things. They should directly observe the neighborhood’s layout, public facilities, housing, and sanitation infrastructure. Nurses should access statistics and records from public health departments, libraries, or local governments to gather demographic information.And they visit community sites such as schools, health facilities, and volunteer organizations to understand available services and resources.
Applying Community Assessment to Individual Care
Nurses can enhance their assessments of individual patients once they have a better understanding of the larger community environment. When the nurse is checking a patient’s home environment, they need to consider many factors like lock safety and illumination, local crime rates, and the cost of emergency services. In addition to keeping themselves informed about neighborhood services like food banks and shelters, nurses can successfully link at-risk patients to the support networks they need.
Importance of Community Assessment
Using community assessments, nurses can create focused health treatments and promote health policies that cater to the needs of particular communities. Nurses can provide culturally appropriate, easily accessible, and long-term health solutions by taking seriously the health of everyone within the framework of the community.
