Cultural Competence in Healthcare
Cultural competence is a critical component of providing effective, patient-centered healthcare in today’s diverse societies. It involves understanding how cultural influences shape health beliefs, practices, and perceptions of illness, as well as recognizing health disparities and social determinants that impact patient outcomes. By developing cultural competence, healthcare providers can better align their care with patients’ values and needs, fostering trust and improving the quality of care. This section explores the steps toward cultural competence, the use of cultural assessments, and the role of equity-focused quality improvement in reducing disparities and ensuring inclusive, respectful healthcare for all.
By the end of this section, you should know about:
- The cultural influences on health and illness.
- How the many facets of culture affect a health care provider’s ability to provide culturally congruent care.
- The health disparities and social determinants of health.
- The steps toward developing cultural competence.
- The relationship between cultural competence and patient-centered care.
- The cultural assessment to plan culturally competent care.
- The research findings applicable to culturally competent care.
- The research finding applicable to equity-focused quality improvement.
- Health Disparities vs. Health Care Disparities
- Health Care Disparities
- Cultural Factors and Health Differences
- Cultural Competence in Healthcare
- Core Measures and Equity-Focused Quality Improvement (QI)
Let’s take a closer look at them.
Test Your Knowledge
At the end of this section, take a fast and free pop quiz to see how much you know about Cultural Competence.
Cultural Competence in Health and Illness: Understanding Cultural Influences.
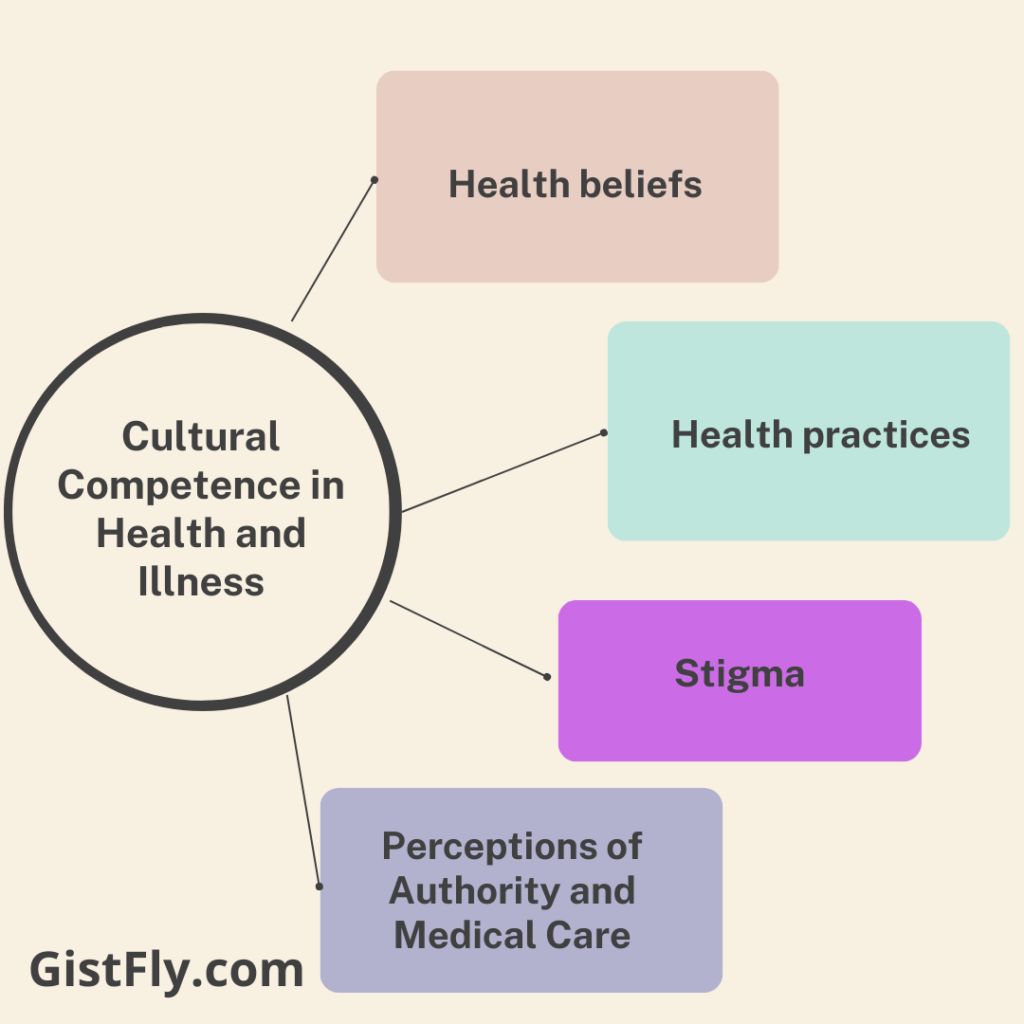
Cultural influences significantly shape how individuals understand and experience health, illness, and healthcare. These influences may include:
Health beliefs: Different cultures have specific beliefs about the causes of illness, such as whether it is physical, spiritual, or the result of lifestyle. For example, some cultures believe that spiritual factors if it causes disease, while others see disease as a natural phenomenon.
Health practices: Cultural traditions influence how people seek medical help, what treatments they use, and when they seek care. For example, some cultures prefer herbal or traditional medicine to modern medicine, which if not accepted can affect treatment effectiveness
Perceptions of Authority and Medical Care: Some cultures may have more respect for authority, including doctors and nurses, while others take a more collaborative approach to health care decisions. The way a patient views his or her doctor or nurse may affect adherence to medical advice and treatment plans.
Stigma: In some cultures, certain health conditions, such as mental illness or HIV, are associated with stigma.
Culture: Culture refers to the shared values, beliefs, customs, practices, and social behaviors of a particular group of people. It includes aspects like language, religion, food, family roles, and health practices that influence how individuals perceive and respond to health and illness.
Cultural Competence in Culturally Congruent Care: Facets of Effective Care
Cultural competence involves recognizing and understanding the diverse cultural factors that can affect the healthcare experience, and adapting care to meet the unique needs of patients. The facets of culture that impact a healthcare provider’s ability to provide culturally congruent care include:
Language and communication strategies: Differences in language or languages, and communication preferences (e.g., direct vs. indirect) can create barriers to understanding and reliability This requires bilingual interpreters or staff and communication strategies clearly apply.
Cultural norms and values: Practices of gender roles, family structure, and the role of the individual in health care decision-making can influence how patients engage with their care. For example, some cultures allow family members to make health care decisions, while others prioritize individual autonomy.
Health literacy: Cultural differences in education, language skills, and understanding of medical terminology can affect a patient’s ability to follow medical instructions. Developing information that is culturally appropriate for the patient is critical to what will result in compliance and health outcomes.
Biases and stereotypes: Unconscious biases and misconceptions about patient culture can influence nurse care decisions, leading to misunderstandings or inequitable care Providers need to be independent recognizing and engaging in reflective practices to overcome biases.
Culturally Congruent Care: Culturally congruent care is healthcare that is tailored to the patient’s cultural needs, preferences, and values. It involves providing care that respects the patient’s cultural context, promoting better health outcomes, and enhancing patient satisfaction.
Cultural Competence, Health Disparities, and Social Determinants of Health
Health Disparities: Health disparities refer to preventable differences in health outcomes and access to healthcare services among different populations. These disparities are often the result of factors like socioeconomic status, education, race, ethnicity, and geography. For example, certain racial or ethnic groups may have higher rates of chronic diseases like hypertension or diabetes due to socioeconomic or environmental factors.
Social Determinants of Health (SDH): These are the conditions in the places where people live, learn, work, and play that affect a wide range of health risks and outcomes. Key SDH include:
Access to healthcare: Availability of affordable health services in underserved areas.
Education and literacy: The level of education can affect a person’s ability to understand health information and make informed health decisions.
Economic stability: Employment, income, and housing stability significantly impact a person’s health.
Social and community context: Social support networks and community engagement influence mental health and access to resources.
Neighborhood and built environment: Safe housing, clean air, and access to healthy food contribute to overall health.
Addressing social determinants of health is crucial in reducing health disparities and improving public health.
Definition of health disparities
Health disparities are defined by Healthy People 2020 as “health disparities that are significantly associated with social, economic, and/or environmental problems” (USDHHS, 2015). They represent inequalities or disparities in health between disadvantaged groups (e.g., low-income individuals) and disadvantaged groups (e.g., low-income individuals) These disparities lead to diseases, injuries, and violence rates are higher among disadvantaged populations relative to their size (CDC, 2013) he wrote.
Causes of health disparities in Cultural Competence
Health disparities result from a complex interplay of factors, including individual genetics and behaviors, public health policies, neighborhood and environmental effects, and health care quality (United Health Foundation, 2014). Community context, and access to social institutions (McGovern et al., 2014). The World Health Organization (2013) emphasizes that social determinants are the conditions in which people are born, grow, live, work and age, driven by global, national and local distributions of resources.
Social Determinants of Health: Social determinants of health are the conditions in which people are born, grow, live, work, and age, and which affect their health outcomes. These determinants include factors like income, education, employment, social support, and the physical environment. Disparities in these social determinants often lead to health inequalities.
Steps Toward Developing Cultural Competence
Developing cultural competence involves gaining knowledge, skills, and awareness to provide effective care to patients from diverse cultural backgrounds. Key steps include:
Self-knowledge and reflection: Identify your own cultural biases, beliefs, and assumptions. Consideration of personal biases helps healthcare professionals improve their interactions with diverse patients.
Cultural knowledge: Know the culture, traditions, and health beliefs of the population you serve. This includes understanding language barriers, religious practices, and customs related to health.
Cultural skills: Develop the ability to analyze cultural factors affecting health, including how to conduct cultural assessments, and incorporate this information into plans of care.
Encounters of Cultural: Engage in meaningful communication with patients from diverse backgrounds to better understand their needs and expectations.
Cultural desire: Demonstrate a willingness and commitment to learn from patients and colleagues from diverse backgrounds, to provide compassionate and efficient care.
Cultural Assessment: Cultural assessment is the process of evaluating a patient’s cultural background, beliefs, values, and practices to better understand how culture impacts their health behaviors, treatment preferences, and healthcare needs. This assessment helps healthcare providers deliver more effective and personalized care.
Cultural Competence and Patient-Centered Care
It is known that Cultural competence is directly related to patient-centered care because it ensures that care is tailored to the individual’s cultural beliefs, values, and preferences. Patient-centered care focuses on the individual needs and preferences of patients, respecting their cultural backgrounds while providing quality care. This means:
Shared decision making: Involving the patient in health care decisions that respect their cultural preferences and values.
Respecting diversity: Identifying and addressing cultural, social and personal factors that influence patient care.
Individualized care: Recognizing that each patient is unique, we tailor care plans to their cultural needs, ensuring a holistic approach to care.
Using Cultural Assessment to Plan Culturally Competent Care
Cultural assessment is important in identifying cultural factors that may affect the care process. These surveys ask patients about their health beliefs, values, language preferences, and family dynamics. The cultural assessment may include questions such as:
What language do you want to speak?
What cultural or religious practices are important to you when it comes to health?
How do you view the role of family in your health decisions?
Are there health beliefs or practices that I need to know to help with your care?
This information helps healthcare professionals plan care that is respectful of the patient’s culture, which can improve patient outcomes and satisfaction.
Research Findings Applicable to Culturally Competent Care
Research has shown that culturally competent care leads to improved patient satisfaction, better clinical outcomes, and reduced healthcare disparities. Some key findings include:
Cultural competence training: Providers who receive cultural competency training are more likely to have positive attitudes toward diverse patients and provide more effective care.
Language services: The use of professional interpreters significantly reduces misunderstandings and improves patient comprehension, particularly for those with limited English proficiency.
Patient-provider relationships: Culturally competent care fosters trust and better communication, which can lead to better adherence to treatment plans and health behaviors.
Cultural Competency: Cultural competency refers to the ability of healthcare providers to understand, appreciate, and effectively interact with patients from diverse cultural backgrounds. It involves knowledge, skills, and attitudes that enable providers to recognize cultural differences, reduce biases, and deliver respectful and relevant care.
Research Findings Applicable to Equity-Focused Quality Improvement
Equity-focused quality improvement initiatives aim to reduce disparities in care by addressing factors such as race, ethnicity, gender, socioeconomic status, and geography. Key research findings include:
Stratified data analysis: Hospitals and healthcare systems that analyze patient data by race, ethnicity, and other social determinants of health are more likely to identify and address disparities in care.
Bias and stereotype reduction: Programs that help providers recognize and manage implicit biases lead to more equitable treatment of minority populations.
Access to care: Expanding access to healthcare for underserved populations (through telemedicine, mobile clinics, and community health workers) improves health equity and outcomes.
Health Disparities vs. Health Care Disparities
Health disparities: refers to differences in the incidence, prevalence, and outcomes of health conditions among different populations.
Disparities of Health are associated with differences in the availability, accessibility, and quality of health services, including screening, diagnosis, treatment, and management.
Access to Health Care
Lack of access to poor health care is a major social determinant of health disparities. Routine primary visits are effective in improving preventive care, but racial and ethnic minorities, such as African Americans, Asians, and Hispanics, are less likely to attend routine primary clinic visits compared to non-Hispanic whites to a (AHRQ, 2013a). Similarly, low- and middle-income groups face more significant barriers to care compared with higher-income groups, and uninsured individuals are less likely to do so permanent primary caregiver In addition, research shows that certain LGBT minority groups have higher rates of chronic health conditions compared to heterosexual populations, and early onset disability high (Ranji et al., 2015).
The Role of Health Care Systems
Health care systems can contribute to disparities through inadequate resources, poor patient-provider communication, lack of culturally competent care, fragmented care delivery, and limited language services (NQF, 2012). The Institute of Medicine (IOM) states that quality care should be safe, effective, patient-centered, timely, efficient, and equitable. However, while U.S. healthcare has improved in many areas, equity remains a persistent challenge (Mutha et al., 2012).
Impact of Health Disparities
The health system can contribute to disparities through inadequate resources, poor patient-provider communication, lack of culturally appropriate care, fragmented care delivery, and unlimited language use (NQF, 2012). The Institute of Medicine (IOM) states that quality care should be safe, effective, patient-centered, timely, efficient and fair. However, although health care in the US has improved in many areas, equity remains a persistent challenge (Mutha et al., 2012).
Health Care Disparities: Health care disparities refer to differences in the quality of care and health outcomes experienced by different populations, particularly those based on race, ethnicity, socioeconomic status, gender, disability, or other social factors. These disparities often result in certain groups receiving poorer care and experiencing worse health outcomes.
Addressing Health Care Disparities
The United States is experiencing a major demographic shift. By 2050, racial and ethnic minorities will make up 50% of the population. The population aged 65 and older is also growing rapidly, from 44.7 million in 2013, and is expected to double by 2060 (Administration on Aging, 2014) Poverty remains a significant issue, in African- For the Americans. Native Americans, Hispanics, and Native Americans have the highest rates (U.S. Census Bureau, 2013). Compounding these challenges, the 2003 National Adult Literacy Survey found that only 12% of U.S. adults were proficient in understanding basic health information (NCES, 2006).
Complexities of Health Care Delivery
The increasing diversity of the U.S. population, including religious orientation, sexual orientation, and gender differences, exacerbates the complexity of the health care system.
Efforts to Address Disparities
Organizations such as the Joint Commission (TJC), National Quality Forum (NQF), and National Commission on Quality Assurance (NCQA) are working to eliminate disparities by promoting:
Cultural Competency: Tailoring care to the unique needs of diverse populations.
Health Literacy: Ensuring patients fully understand their health needs.
Patient- and Family-Centered Care: Engaging patients and families to improve care quality and reduce disparities.
Health Disparities in the United States
Health disparities in the US. is due to a variety of social, cultural, and economic factors. This disparity includes groups based on racial or ethnic identity, religion, socioeconomic status, sex, age, mental illness, mental or physical disability, sexual orientation or gender, and location. Historical discrimination and systemic discrimination often exacerbate these disparities, leading to health outcomes for marginalized groups.
Marginalized Groups: Marginalized groups are populations that are pushed to the edges of society and experience social, economic, and political disadvantage. These groups may include racial and ethnic minorities, LGBTQ+ individuals, people with disabilities, immigrants, and those living in poverty. They often face systemic barriers to healthcare, education, and economic opportunities.
Cultural Factors and Health Differences
Culture plays an important role in health disparities by influencing values, beliefs, and practices. Research highlights disparities in health conditions such as cancer, diabetes, infant mortality, and organ transplantation among different cultural groups, for example, African Americans have the highest cancer mortality, while Asian Americans have a disproportionately high incidence of liver cancer. Hispanic youth are at increased risk for obesity, increasing their chances of developing chronic conditions such as diabetes and asthma. These differences emphasize the importance of addressing cultural factors in health care.
Discrimination and Health Inequities
Discrimination based on sexual orientation and gender identity significantly impacts mental and physical health. Gay, lesbian, and bisexual youth are at higher risk for depression, anxiety, and substance abuse, and they are four times more likely to attempt suicide compared to heterosexual peers. Transgender individuals often delay seeking medical care due to discrimination and lack of insurance, further compounding health inequities.
Infant Mortality Disparities
Infant mortality in the United States shows significant differences across cultural groups. American Indian and Alaska Native populations experience rates 60% higher than non-Hispanic whites, while African American babies experience more than twice the white infant mortality Alarmingly, even highly educated African American women face higher infant mortality rates compared to similarly educated white women are, reflecting systemic inequalities than socio-economic factors.
Understanding Culture and Intersectionality
Culture includes values, norms, and traditions passed down from generation to generation. Historically associated with ethnicity, race, nationality, and language, culture now includes gender, sexual orientation, class, and immigration status Intersectionality—social categories such as race, gender, and overlapping classes—redetermine how these components combine to form individuals. access to resources, including health care.
Key Concepts in Intersectionality
Social Inequality: Certain groups face limited access to essential services.
Marginalization: Exclusion from political and economic opportunities reinforces disparities.
Social Location: A person’s societal position, defined by group memberships, influences their resource access.
Matrix of Domination: Social identities must be understood within broader systems of power and privilege.
Adopting an intersectional perspective enables healthcare providers to address systemic inequities effectively.
Intersectionality: Intersectionality is a concept that explores how different aspects of a person’s social and identity categories (such as race, gender, class, sexuality, ability, etc.) intersect to create unique experiences of discrimination or privilege. It recognizes that individuals are affected by multiple social identities simultaneously, and that these intersecting identities can affect their access to resources and opportunities.
Cultural Competence in Healthcare
Leininger’s transcultural nursing emphasizes understanding and integrating patients’ cultural values and life patterns into care. Personalized healthcare considers individual beliefs, habits, and lifestyles rather than imposing standardized approaches. For example, understanding a Muslim patient’s preference for female healthcare providers can ensure respectful and effective care.
The Role of Nurses in Cultural Competence
Nurses play a crucial role in delivering culturally congruent care by:
- Collaborating with patients and interdisciplinary teams.
- Continuously learning about cultural differences to provide tailored support.
- Respecting individual preferences and adapting care practices accordingly
Teach Back Technique
A Teach Back method is a communication tool designed to confirm patients’ understanding of information provided by healthcare professionals. It attempts to clarify by asking patients to reinterpret the information in their own terms rather than evaluating it. This leads to “Do you understand?” which can lead to misunderstandings. Effective questions include open-ended questions such as “Please explain back to me so I can make sure I give you the information you need”. Or “How would you make this change at home?”. Use the teach back technique in a non-embarrassing way, and create a comfortable environment for patients to express their understanding. Healthcare professionals should view this approach as an opportunity to test their communication skills rather than analyzing the patient. Practical tips for using teach back effectively include developing a strategy. Using visual aids to reinforce instructions, clarifying any misunderstandings, and practice until it becomes routine.
Cultural Encounters and Cultural Desire
Intercultural encounters involve direct contact with patients from different cultures. fostering therapeutic relationships, and helping healthcare professionals refine their values and practices. These contacts can also help resolve intercultural conflicts, foster understanding development. And improve patient outcomes by respecting patient and nurse perspectives willingness to meet the needs of diverse patients. Identify the provider give her the personal motivation to engage in culturally appropriate care driven by genuine interest and compassion. This desire helps overcome challenges like time constraints or discomfort. making cultural competence an essential aspect of ethical and responsible care.
Cultural Competence in Healthcare Organizations
Health policy plays an important role in promoting cultural competence through staff training, ensuring adequate interpreter services, and incorporating health literacy into communication practices. Policy should include a broad definition of family planning about and collect demographic data. This is to identify and address disparities in care. Organizations should use hierarchical outcomes data to improve diversity of care, while demonstrating a commitment to equity and inclusion. Nurses can be advocates for change to ensure that institutional policies support culturally appropriate care and nurture patients.
Transcultural Nursing: Transcultural nursing is a field of nursing that focuses on providing culturally competent care to patients from diverse cultural backgrounds. It emphasizes the need for nurses to understand and integrate cultural differences into their practice to ensure that care is appropriate and respectful of patients’ cultural beliefs and practices.
Worldview: Worldview refers to the overall perspective from which an individual or group interprets the world and their place in it. It encompasses beliefs, values, and assumptions about reality, life, and existence. A person’s worldview is shaped by factors such as culture, religion, education, and personal experiences and influences how they approach health, illness, and healing.
Core Measures and Equity-Focused Quality Improvement (QI)
Key initiatives developed by organizations such as The Joint Commission (TJC) and the Centers for Medicare and Medicaid Services (CMS) are evidence-based quality indicators aimed at improving health care outcomes and reducing costs. These products target conditions such as heart disease, myocardial infarction, pneumonia, and so on. Equity-focused QI seeks to reduce disparities among racial, ethnic, and socioeconomic groups and emphasizes customized interventions to meet the needs of vulnerable populations. Steps include collecting data by race and ethnicity, integrating equity into QI programs, evaluating and refining interventions, and continuously improving over time Primary care nurse use participates in QI efforts to address disparities and improve outcomes for underserved populations.
Patient Care and Communication Frameworks
Addressing social determinants of health is vital to understanding patient challenges. Factors such as socioeconomic status, housing instability, and lack of access to healthcare can significantly affect patient outcomes. Communication frameworks like C-LARA (Control, Listen, Acknowledge, Recommend, Assess) help foster empathetic, supportive interactions. For instance, actively listening to a patient’s concerns and acknowledging their experiences can build trust. Additionally, open avenues for effective recommendations.
Overcoming Barriers in Patient Care in Cultural Competence
Weight issues, treatment nonadherence, and repeated emergency department (ED) visits are common challenges in managing chronic conditions. Healthcare providers must identify the underlying barriers—such as financial constraints, stress, or lack of resources. while avoiding biases or assumptions about a patient’s motivation or capabilities. Self-awareness helps providers approach these situations with empathy. Ensuring that care plans are tailored to the patient’s unique needs and circumstances.
Nursing’s Role in Quality Improvement
Nurses are central to improving care quality and reducing disparities by addressing gaps in care and advocating for changes in policies and practices. Using evidence-based methods like Teach Back ensures that patients understand their care plans, particularly after discharge. Assessing social determinants, arranging follow-ups, and leveraging predictive analytics tools can help identify high-risk patients and improve self-management, reducing readmission rates. By engaging in QI initiatives, nurses ensure that care is safe, effective, and equitable.
Explanatory Model: An explanatory model is a framework used by healthcare providers to understand how a patient perceives the cause, course, and treatment of their illness. This model incorporates the patient’s cultural beliefs and can be crucial in ensuring that healthcare interventions are aligned with the patient’s understanding of their condition.
