Evidence-Based Practice
Evidence-Based Practice (EBP) empowers nurses and other professionals to deliver care that integrates the best available evidence. By integrating clinical expertise, patient preferences, and the latest research, Evidence-Based Practice (EBP) informs healthcare decisions, making them effective and aligning them with the highest standards of practice. This approach not only improves patient outcomes but also fosters continuous learning and innovation within the nursing profession.
By the end of this section, you will know about:
- The benefits of evidence-based practice.
- The steps of evidence-based practice.
- PICOT question.
- The levels of evidence available in the literature.
- Ways to apply evidence in practice.
- Nursing research and improving nursing practice.
- The steps of the research process.
- Priorities for nursing research.
- The relationship between evidence-based practice and performance improvement.
Let’s take a closer look at them.
Test Your Knowledge
At the end of this section, take a fast and free pop quiz to see how much you know about Evidence-Based Practice.
The benefits of evidence-based practice
Modern health care requires nurses to provide quality and cost-effective care. Besides, evidence-based practice helps providers like Rick make informed decisions at the right time, improving patient outcomes, safety, and satisfaction, while reducing costs. By integrating EBP, nurses meet professional, political, and social imperatives to improve health care.
Benefits of Evidence-Based Practice
EBP enables nurses to make clinical decisions based on the best available evidence, knowledge, and patient preferences. For example, Rick’s idea of evidence-based management of postoperative pain is consistent with this approach, directly improving the quality of care. Overall, Healthcare organizations expect EBP and requires ongoing education and practice at the bedside.
Sources of Evidence-Based Practice
EBP provides a variety of resources such as textbooks, nursing journals, health care databases, improvement information, infection prevention statistics, and clinical expertise aimed at achieving better information most, cutting-edge, and appropriate for effective patient care.
Difficulties in obtaining evidence.
In practice, practitioners often lack access to simple scientific literature, relying instead on traditional or simplistic sources. Systematic reviews, when well-designed, provide the most reliable evidence. Rick’s approach to music therapy research is an example of how hard evidence is sought about non-research-based practices.
Importance of patient-based management.
Even the best evidence is not universally applicable, as patient values, preferences, and circumstances influence care decisions. Nurses must use critical thinking to adapt the evidence to the specific needs of each patient, ensuring safe and effective care tailored to the individual expectations.
The steps of evidence-based practice
The seven-step, structured problem-solving program integrates evidence into patient care.
1. Cultivate a Spirit of Inquiry
Nurses must actively question existing practices and seek knowledge that will improve patient outcomes. Commitment to EBP results in high quality care and requires a supportive health care environment that encourages questioning and continuous improvement.
2. Ask a Clinical Question in PICOT Format
Nurses need to be aware of specific clinical questions, usually based on practical challenges or trends noted in patient care. The PICOT (patient/problem, intervention, comparison, outcome, time) framework refers to the assessment and accumulation of evidence, to better frame these questions.
3. Search for the Best Evidence
It is important to identify the most relevant and scientifically sound evidence. Research in scientific journals generally provides the most reliable data, supporting high quality patient care.
4. Critically Appraise the Evidence
Practitioners should assess the quality, relevance and validity of collected evidence to ensure its appropriateness to the clinical setting. Research helps determine whether the evidence is reliable enough to implement new practices.
5. Integrate Evidence with Clinical Expertise and Patient Values
Combining research evidence with nursing expertise and understanding patient preferences ensures that decisions are scientifically informed and patient-centered, resulting in optimal outcomes.
6. Evaluate Practice Changes and Outcomes
Once EBP-based changes have been implemented, it is important to measure their effectiveness to ensure that the desired outcomes are achieved. This study highlights how the changes improve patient care quality and safety.
7. Share Outcomes with Others
Healthcare providers adopt successful practices across different settings by using the results of EBP-based improvements.
Formulating Clinical Questions with PICOT
Identifying Knowledge Gaps: PICOT questions help narrow down specific practice areas that need evidence-based solutions.
Examples of PICOT Questions:
- Does a smaller gauge IV needle prevent blood cell damage when administering PRBCs?
- Is an adult patient’s blood pressure more accurate with feet flat versus crossed?
PICOT question: A specific question format used in EBP to guide research and clinical inquiry. PICOT stands for Population, Intervention, Comparison, Outcome, and Time, helping structure questions to identify relevant evidence for practice changes.
The levels of evidence available in the literature
The sequence of evidence strengthens how findings are applied and ensure their reliability in nursing practice. In the order of systematic reviews and meta-analyses, which provide the highest level of evidence at the top of the hierarchy. Meta-analyses use statistical methods to quantify the effects of interventions, whereas systematic reviews pool studies without statistical conclusions. Moreover, Randomized controlled trials (RCTs) are considered the gold standard for accurate and reliable results, with reviews of multiple RCTs providing more robust evidence. Other sources of evidence are research studies, quality improvement information, clinical guidelines, infection prevention information, and expert opinion. Nurses also rely on searchable databases such as AHRQ, CINAHL, MEDLINE, and Cochrane to find peer-reviewed research.
Clinical guidelines: Evidence-based recommendations that guide healthcare professionals in the treatment and care of patients. These guidelines are developed from rigorous research to provide best practices in managing specific health conditions or procedures.
Peer-reviewed: A process by which scholarly articles and research are evaluated by experts in the field before publication. Peer review ensures that research meets high standards of quality, accuracy, and scientific rigor.
Reliability: The degree to which a research method produces consistent and repeatable results. Reliable studies yield similar findings when repeated under the same conditions.
How to apply evidence in practice?
Integrating patient care: Strong evidence such as findings from systematic reviews or meta-analyses can directly inform patient care practices or guide policy innovation.
Critical thinking and individualization: Evidence must be tailored to the specific needs and preferences of individual patients. Nurses must balance scientific findings with patient values and context, and use critical thinking to ensure consistency with care expectations.
Pilot studies: When evidence is insufficient or context-specific, exploratory studies can be conducted to gather more data and help refine the implementation of interventions.
Ongoing evaluation: Evaluate the effectiveness and safety of implemented changes. If unexpected outcomes, such as increased complications, occur, the process may need to be re-evaluated.
Education and training: Provision of resources such as EBP councils, journal groups, and databases that, keep practitioners up to date on the latest evidence and best practices.
Sharing: Sharing results through presentations or publications increases the acceptability of effective practices, contributing to the overall improvement of nursing knowledge.
Nursing research and improving nursing practice.
Nursing research is a foundation for advancing knowledge in the profession, improving patient care, and providing better healthcare resources. Also, research of nursing that focuses on evidence-based practice provides scientific support for effective interventions, which helps validate nurses’ contribution to patient health outcomes Pattern major in this area was Dr. Norma Matheny’s study of aspiration prevention in tube-feeding patients, which directly affected medical practice, so that in patients Risk of complications is reduced.
Nursing research: Systematic investigation aimed at generating new knowledge specifically to enhance nursing practices and improve patient outcomes. Nursing research focuses on issues relevant to patient care and healthcare delivery.
Outcomes Research and Care Delivery in Evidence-Based Practice
Outcomes research is needed to assess the true impact of health interventions on patients. It typically examines the effectiveness, risks, and costs of treatments. For that reason, this type of research is important because it informs patients, health care providers, and policymakers, and ensures that clinical decisions are consistent with current evidence. For example, research on telemedicine for Parkinson’s disease has shown how access to care can be improved for specific patients. In nursing, outcomes such as patient satisfaction or health status are indicators of the effectiveness of care delivery, particularly nurse-sensitive indicators such as the quality of nursing care.
The Scientific Method in Nursing Research
The scientific method is an organized foundation for reliable nursing research. Researchers follow a set of steps to ensure the validity and objectivity of their findings. Important characteristics are clear identification of research questions, control of external factors, collection of empirical data, and objective generalization of findings to a broader population This approach is helpful to researchers for reducing bias, maintaining consistency, and obtaining results that can influence practice.
Research in Evidence-Based Practice
Nursing assessments include various types, broadly divided into quantitative and qualitative approaches:
Quantitative research focuses on measurement accuracy and statistical data. Examples are:
- Experimental research: includes randomized controlled trials (RCTs) that rigorously test interventions.
- Non-experimental research: involves observational research that describes relationships between variables.
- Survey research: collects large amounts of data, usually about attitudes or traits in a population.
- Research evaluation: evaluates the effectiveness of programs or interventions.
Qualitative research examines psychological phenomena such as patient experiences, which are often difficult to quantify. This method of research, which involves interviews or observations, helps to understand context and individual perspectives on health issues. Common methods include ethnography, phenomenology, and grounded theory.
Implications for nursing practice
Understanding nursing research is important for nurses who want to base their practice on evidence rather than emotion or behavior. Evidence-based practice includes questioning traditional approaches and exploring whether there are more effective interventions for specific patient populations. Research findings also need to be widely disseminated to influence practice in different settings.
Bias: A distortion or deviation in results or findings that can occur in research, often due to researcher influence, participant selection, or methodological flaws. Bias can affect the accuracy and validity of a study’s results.
Empirical data: Data obtained through direct observation, experimentation, or experience rather than through theory alone. Empirical data provide objective evidence and form the foundation for scientific conclusions.
Qualitative nursing research: A research approach that explores the experiences, beliefs, and feelings of patients and healthcare providers through non-numeric data. Qualitative methods often include interviews, focus groups, and observations.
Quantitative nursing research: A research approach that focuses on collecting and analyzing numerical data to quantify variables and determine relationships or differences. This type of research uses statistical methods to draw conclusions.
Scientific method: A structured process of inquiry that involves observing, hypothesizing, experimenting, and analyzing to answer questions or test theories systematically. The scientific method ensures that findings are objective and reproducible.
Validity: The extent to which a study accurately measures what it intends to measure. Valid research provides trustworthy and credible findings that genuinely reflect reality.
Variables: Elements, traits, or conditions that researchers manipulate, measure, or control in a study. Variables can be independent (causing change) or dependent (affected by other variables), and they are key in determining relationships in research.
The steps of the research process
The research process is a process of answering research questions, from identifying the problem to finding answers, and often leads to new questions This process generates knowledge that is applied to similar situations and generates action evidence-based is greater in areas such as nursing.
Example of a research study in nursing
In the example provided, a nurse investigates whether chewing peppermint tablets after colon surgery reduces constipation and speeds bowel movements This study is foundational to the use of research materials in nursing in the real situation.
Steps in the Research Process
The assessment process begins with identifying the problem. In this scenario, a nurse notices that postoperative nausea is common in patients after spinal surgery. After consulting with a researcher, the nurse formulates a question about whether peppermint chewing gum alleviates constipation or improves bowel function and recovery. The literature review reveals a paucity of existing research on this particular phenomenon.
The next step involves developing research questions and hypotheses. Based on the identified problem, the nurse creates questions and hypotheses to guide the study’s design. Planning the study follows, focusing on study design and methodology. The researchers assign patients randomly to either a control group receiving standard care or an experimental group receiving standard care plus gum chewing. The sample is limited to elective colon resection patients, excluding emergency cases. The independent variable is gum chewing, while dependent variables include nausea levels and bowel function recovery markers such as bowel sounds, passing gas, and the first bowel movement. Data collection tools are chosen to measure nausea and track recovery times through patient assessments and charts.
In sum, moral considerations are paramount. The research team obtains Institutional Review Board (IRB) approval to ensure support for ethical standards. Researchers provide informed consent to participants to ensure they understand the study’s purpose, procedures, potential risks, and benefits. The researchers guarantee voluntary participation and ensure confidentiality.
More steps
Data are collected as standardized during assessment, and unit nurses check for bladder and bowel resuscitation. The review team ensures that all reviewers adhere to protocols to maintain consistency. The research team analyzes the data. While statistics help the team is testing whether oral chewing significantly affects the recovery of bladder and bowel function. Study limitations have been identified, such as the small sample size (20 patients per group) and inconsistent patient chart documentation, which limit the generalizability of the findings.
The findings are applied to nursing practice. Based on positive results, the team recommends the addition of peppermint extract as part of postoperative care for spine surgery patients. Recognizing the limitations of the study, further studies are recommended to investigate the efficacy of this intervention in other abdominal surgeries. Researchers disseminate the results of the study through presentations and publications to inform healthcare professionals and influence postoperative care practices.
Confidentiality: The ethical principle that ensures information about study participants is kept private and only accessible to authorized individuals. It protects participants’ identities and personal information from unauthorized disclosure.
Generalizability: The extent to which study findings can be applied to broader populations beyond the sample studied. High generalizability means the results are likely applicable to similar groups in different settings.
Hypotheses: Statements predicting a relationship between variables. Hypotheses guide the research process by providing a clear focus for investigation, and they are tested through empirical study.
Informed consent: A process in which researchers provide study participants with comprehensive information about the study, including its purpose, procedures, potential risks, and benefits. Informed consent ensures that participants voluntarily agree to participate with full understanding.
Research Process: An organized series of steps that researchers follow to answer specific questions or investigate a problem. It typically includes identifying a problem, reviewing literature, designing a study, collecting data, and analyzing results.
Priorities for nursing research.
The relationship between evidence-based practice and performance improvement.
Overview of Evidence-Based Practice, Research, and QI
EBP, research, and QI are interrelated processes that share the goal of improving patient care by utilizing the best available evidence. As a nurse, understanding these processes is crucial to choosing the right approach for clinical issues and improving patient care outcomes.
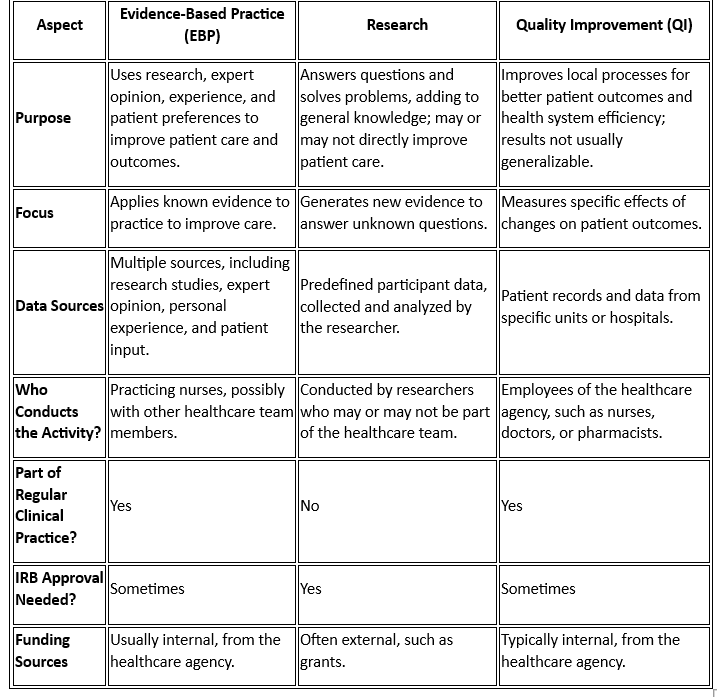
Key Differences and Similarities Among Evidence-Based Practice, Research, and QI
Example of Evidence-Based Practice, Research, and QI in Action
- Problem Identification: A group of nurses note a decrease in patient satisfaction with pain management.
- Quality improvement (QI) data analysis: QI data refer to policies related to pain management (e.g., types of pain medications prescribed, patient response to pain management).
- EBP implementation: The unit’s quality council team reviews the literature and identifies the best evidence to enhance patient quality pain management programs in the unit. After implementation of the modified system, the results are analyzed.
- Conduct a survey: If patient satisfaction with pain management is still low, the team can then conduct a survey to further examine the problem and develop solutions to improve patient care.
Explain the Relationship Between Evidence-Based Practice and Performance Improvement (PI)
Evidence-based practice and performance improvement are closely linked as they both aim to enhance healthcare quality:
- EBP uses research findings to inform clinical decisions and best practices. It relies on strong evidence to support specific interventions and patient care strategies.
- Performance Improvement (PI) focuses on evaluating and optimizing current healthcare processes and practices within an organization to achieve better outcomes.
Performance Improvement (PI): An approach focused on improving processes within an organization to enhance patient outcomes and operational efficiency. Unlike research, PI is often internally focused and does not seek to generate generalizable knowledge.
