Health and Illness
In this section, we will delve into the critical aspects of health and illness, exploring how risk-factor modification and behavior change can promote wellness. You’ll learn about the variables that influence how individuals respond to illness, the impact of illness on patients and their families, and the essential role nurses play in supporting health and managing illness. Let’s take a closer look!
By the end of this section, you will know about:
- Risk-factor modification and changing health behaviors.
- Variables influencing illness behavior.
- The effect of illness on patients and families.
- A nurse’s role in health and illness.
Let’s take a closer look at them.
Test Your Knowledge
At the end of this section, take a fast and free pop quiz to see how much you know about Health and Illness.
Risk-factor modification and changing Health and Illness behaviors.
Identifying and addressing risk factors through behavior change is central to health promotion and illness prevention. A comprehensive nursing assessment helps identify health hazards and risk factors for each patient. Once these risks are identified, nurses engage patients in decision-making about maintaining or improving their health through specific risk-reduction actions. Changing unhealthy behaviors, especially those deeply ingrained in lifestyle patterns, is often challenging, but the nurse’s role in facilitating change is essential.
Stages of Health and Illness Behavior Change (Transtheoretical Model)
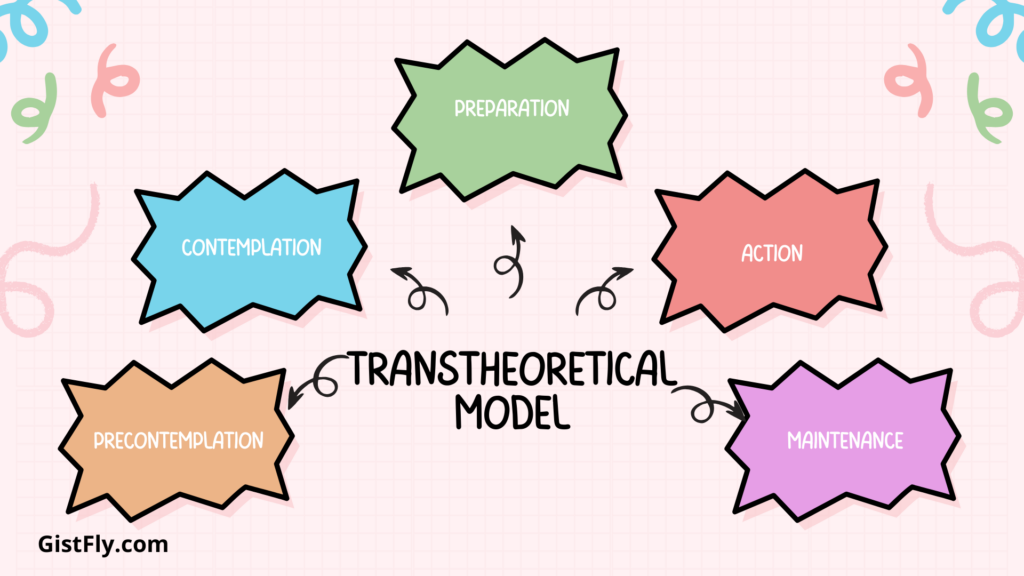
The Transtheoretical Model developed by Prochaska and DiClemente outlines the stages of change people commonly go through when modifying health behaviors. Nurses use this model to guide patients through the process of change by tailoring interventions to each stage:
- Precontemplation:
- Definition: Patients have no intention to change behavior in the near future (within the next 6 months).
- Nursing Implications: Provide information carefully, as patients may be resistant or defensive. Focus on raising awareness about health risks without pushing for immediate action.
- Contemplation:
- Definition: Patients are considering making a change within the next 6 months.
- Nursing Implications: Patients may show ambivalence but are more receptive to information. Nurses can help by discussing the pros and cons of change and building patients’ confidence in the value of change.
- Preparation:
- Definition: Patients are making small changes and planning a significant change within the next month.
- Nursing Implications: Assist in creating a realistic plan and help patients identify the advantages of change, working together to set achievable goals.
- Action:
- Definition: Patients are actively working on changing their behavior, with efforts lasting up to 6 months.
- Nursing Implications: Nurses support patients by identifying and overcoming barriers, reinforcing positive behaviors, and helping maintain motivation.
- Maintenance:
- Definition: The behavior change has been sustained for more than 6 months and is being integrated into the patient’s lifestyle.
- Nursing Implications: Reinforce the importance of maintaining new habits and help prevent relapse by offering continued support and encouragement.
Relapse is common during the change process, and patients may return to earlier stages. Nurses should treat relapse as a learning opportunity, using it to strengthen the patient’s resolve for future attempts.
Variables influencing Health and Illness behavior.
Nurses play an important role in helping patients reduce their health risks by adopting and maintaining best practices. Several strategies can be used to facilitate behavior change corresponding to the stages of change. The key strategy is active listening and sharing information. Nurses begin with patients’ current understanding of their health risks and behaviors. By clarifying misconceptions through open-ended questions, nurses can engage patients and create a supportive environment for learning.
Another important technique is to set goals and create a timeline. Collaborating with patients to set achievable goals is essential, breaking big changes down into small, achievable steps. Establishing a specific timeline provides structure and helps to measure progress, allowing both patient and provider to monitor progress over time. Nurses also work with patients to identify and address barriers to change. These barriers, such as lack of time, resources, or support, can be articulated, and nurses can help identify solutions or suggest alternative ways to overcome these challenges.
Singing culturally and educationally appropriate materials is an effective alternative. Nurses must provide materials that are appropriate for the patient’s reading and culture, and ensure that the information is accessible and relatable. Involving family members in the intervention can also be beneficial, as their involvement provides additional support and encouragement, which can be especially helpful in maintaining lifestyle changes. Finally, positive energy and monitoring is important. Nurses encourage patients to track their progress through tools such as journals or calendars, record activities such as exercise and dietary changes. Regularly reviewing progress, making recommendations, and adjusting processes as needed helps maintain motivation and ensure continued success.
Application of the Health and Illness Belief Model
The Health Belief Model can be applied in various situations, such as when Sandy, a university nurse, designs a measles outbreak risk-reduction program. In this scenario, Sandy would address the perceived susceptibility and severity by educating students about the likelihood and seriousness of contracting measles. She would highlight the perceived benefits of immunization, such as reducing disease spread and preventing complications. Sandy would also focus on addressing perceived barriers, like concerns about vaccine safety or access, by providing accessible information and services. To prompt action, she would use cues to action, such as posters or campus emails, encouraging vaccination. Finally, to boost self-efficacy, Sandy would empower students by providing resources and answering any questions, enabling them to make informed decisions about vaccination.
Evaluation of Behavior Change
To evaluate progress, nurses can engage patients in several ways. First, they can ask patients to demonstrate understanding, having them summarize the steps needed to reduce health risks and share their comprehension of the lifestyle changes required. Nurses can also encourage patients to track their habits, maintaining logs for diet and exercise, and discussing their experiences with adhering to these changes. Lastly, discussing successes and challenges provides valuable insights into what has worked well for the patient and any difficulties encountered. This allows the nurse to provide targeted support, adjust strategies, and reinforce positive behaviors to ensure continued success in behavior change.
Nurses play an important role not only in medicine but also in the personal, social, and emotional impact of illness. Let’s explore the different aspects of the disease, its classification, and its impact on patients and families.
Acute vs. Chronic Illness
Acute illness is usually short-lived, with symptoms that appear suddenly, are severe, and often resolve within a short period of time. Examples include illnesses such as the common cold or a broken bone, they often cause temporary lifestyle changes. In contrast, a chronic illness lasts longer, about six months, and is often irreversible. Chronic conditions such as diabetes or arthritis have a long-term impact on daily life and work Chronic diseases are common, often associated with lifestyle factors, such as lack of physical activity, malnutrition, tobacco and alcohol Provide.
Illness Behavior
Illness behavior refers to how people respond to symptoms, manage their health, and seek care. A patient’s circumstances, cultural background, personal experience, and social norms can all influence his or her illness behavior. For example, a person with the flu may choose to stay home and rest, while another may immediately go to the hospital. By understanding these behaviors, helping patients recognize their symptoms. Providing guidance on when to provide care, nurses can make changes in the approach. Illness behaviors are also a form of coping, and may provide temporary relief from social activities or responsibilities.
The effect of illness on patients and families.
Illness can cause significant emotional and behavioral changes in patients and their families. Affecting body image, self-concept, activities and family dynamics:
• Behavioral and emotional changes: Acute and transient illnesses can cause few problems, while life-threatening situations often elicit complex emotional responses such as anxiety or anger. Nurses role especially helping patients and families deal with these feelings They are inside.
• Effects on body image: Changes due to illness or treatment (e.g., haircuts or hair loss due to chemotherapy) can affect how patients see themselves. Patients often go through a series of transitions, from shock to denial and finally, to acceptance and change. Nurses can assist patients in this journey by addressing body image concerns with empathy.
• Effect on self-concept: The illness can challenge the patient’s image and self-worth, affecting relationships and causing family stress. For example, a mother who is unable to care for herself because of illness may feel guilty or frustrated. Nurses observe and manage changes in self-concept and provide interventions that support psychological well-being.
• Impact on family activities: The illness can disrupt established family activities, sometimes requiring a reversal of activities. For example, an older child may need to take on the role of caregiver for an ill parent, which can cause stress and role conflict. Nurses provide guidance to families to adjust to these changes, providing resources and support as needed.
• Impact on family dynamics: Illness affects family decisions and communication, often causing stress or anxiety. When one family member becomes ill, other members may have their roles, responsibilities, and expectations disrupted. Nurses help families manage these tensions, with the goal of restoring balanced functioning.
The role of nurses in supporting patients and families
Nurses are critical in supporting patients with chronic conditions and supporting families through the complex emotional and social changes of illness. Their work extends beyond treating symptoms to addressing the overall well-being of patients. By providing guidance, education and compassion, nurses enable patients to live healthy lives despite their circumstances and empower families to adapt to their role in supporting each other in times of in the intensity of the match.
A nurse’s role in health and illness
In order to provide appropriate, safe, and compassionate care, nurses must put their own health and well-being first. Because of the complex nature of their work. Nurses are particularly vulnerable to compassion exhaustion, a condition that combines secondary traumatic stress (STS) and burnout (BO) Secondary traumatic stress (STS) occurs during in which nurses develop deep emotional bonds with patients and families. Unlike nurses, who may be most affected by witnessing patients’ suffering, loss, or trauma, leading to symptoms such as anxiety, disturbed sleep, and emotional exhaustion, burnout (BO) is generally material job-related factors. For example job dissatisfaction, conflict in relationships, or feeling overwhelmed. Burns can lead to irritability, chronic fatigue, and an inability to empathize with patients.
Symptoms of compassion fatigue, such as irritability, frustration, and difficulty concentrating, can significantly affect the nurse’s well-being and the nurse’s well-being.
Personal Strategies for Combating Compassion Fatigue
Nurses can take many individual steps to manage and prevent compassion fatigue. Healthy lifestyle choices are important. Maintaining a healthy diet with well-balanced, high-fiber foods can help support both physical and mental fitness. Ensuring adequate and healthy sleep is important for emotional regulation and resilience. In addition, exercise and relaxation techniques such as mindfulness and meditation can help nurses manage stress and maintain energy levels. It’s also important to create a work-life balance; Establishing boundaries between work and personal life prevents overextension and helps maintain psychological well-being.
Access to coping skills and support systems is another important strategy. Nurses can benefit from learning and practicing coping strategies, such as setting aside time to process grief following the loss of a patient. Building a mentoring relationship with an experienced nurse can provide valuable emotional support and guidance. For some, spiritual well-being is important; Engaging in spiritual or meditative practices can provide a sense of purpose and grounding, helping to prevent emotional exhaustion.
Institutional Strategies for Addressing Compassion Fatigue
Health care organizations also play a crucial role in supporting nurse resilience and addressing compassion fatigue. Institutions are increasingly offering educational programs to increase awareness about compassion fatigue, its effects, and prevention strategies. These programs help nurses understand the signs of STS and burnout, empowering them to take proactive steps to safeguard their well-being. Additionally, organizations are providing coping tools such as support groups, debriefing sessions, and counseling, which help nurses manage the emotional and psychological toll of their work. Finally, offering professional support through access to mental health professionals within the organization provides essential resources for nurses dealing with high levels of stress and burnout. By fostering a supportive environment, healthcare institutions can reduce the impact of compassion fatigue and promote nurse well-being.
