Health and Wellness
This section provides an overview of health and wellness concepts, focusing on public health goals, models of health, and the factors that influence health beliefs and practices. You will also explore health promotion, illness prevention strategies, levels of preventive care, and key risk factors affecting health. Let’s dive in!
By the end of this section, you should know about:
- The four general Healthy People 2020 public health goals for Americans.
- The definition of health.
- The health belief, health promotion, basic human needs, and holistic health models to understand the relationship between patients’ attitudes toward health and health practices.
- The variables influencing health beliefs and practices.
- The health promotion, wellness, and illness prevention activities.
- The three levels of preventive care.
- Four types of risk factors affecting health.
Let’s take a closer look at them.
Test Your Knowledge
At the end of this section, take a fast and free pop quiz to see how much you know about Health and Wellness.
The four general Healthy People 2020 public health goals for Americans
Traditionally, health was viewed simply as the absence of disease. Modern approaches, however, recognize health as a complex multidimensional concept that includes the distinction between illness and optimal well-being. This growing understanding underscores the importance of addressing health care as a dynamic and holistic context.
The Role of Nurses in Health and Wellness Research
Nurses play a critical role in patient health using health models to understand the complex relationships between health, well-being, and illness. By assessing patients on an ongoing basis, nurses identify areas that should be improved and potential risks are experienced, enabling the adoption of proactive health care strategies.
The Impact of Nurses on Health and Well-being
Nurses are uniquely positioned to help patients navigate the complexities of the healthcare system and achieve optimal health. They actively promote health, prevent disease, and help patients overcome health challenges. In addition, nurses help keep healthcare costs down and ensure patients have access to advanced technology and resources.
Risk identification and adjustment
An important part of the nursing profession is the identification of real and potential risk factors, which may lead to illness. Nurses develop personalized strategies to help patients adjust to these risk factors, thereby improving overall health and preventing disease.
Understanding disease behavior
Responses to illness called “illness behavior” vary depending on individual psychology and cultural influences. Nurses who understand these responses provide emotional and practical support, helping to reduce the impact of illness on patients and their families. This approach allows patients to maintain or regain optimal function.
The expanding role of nurses in modern health care
As healthcare evolves with rising costs and advanced technology, nurses are becoming increasingly important in improving personal and social health. They take a holistic and preventative approach to health and wellbeing and go beyond treating diseases, emphasizing the importance of addressing the whole person.
Healthy People
The “Healthy People” initiative is an evidence-based, 10-year set of national goals aimed at promoting health and preventing disease in the US. First introduced in 1979, the foundation document, Healthy People: The Surgeon General’s Report on Health Promotion and Disease prioritizes prevention, health promotion and disease prevention.
Healthy People 1990
The goal of the 1979 report was to improve the health of Americans by 1990, including preventive services, health care, health promotion, and risk reduction It emphasized the need that public awareness, health care, safety measures, and evaluation of surveillance research are raised. This strategy shifted the focus from disease care to health promotion and disease prevention, and required collaboration between governments, organizations, businesses and individuals
Healthy People 2000
Published in 1990, this document set specific health reform goals to be achieved by 2000. It emphasized the need for collaborative efforts across sectors to meet the nation’s health priorities emphasize efficiency
Healthy People 2010
Published in 2000, it offered a comprehensive road map for health reform in the first decade of the 21st century. It emphasized the link between individual and community health, emphasizing that community well-being is an integral part of the nation’s overall health.
Healthy People
Approved in December 2010, Healthy People 2020 introduced four overarching goals aimed at ensuring that all Americans live longer, healthier lives:
Get high quality, as long as you don’t get preventable illness, disability, injury and premature death.
To achieve health equity, disparities will be eliminated to improve the health of all groups.
Create a healthy social and physical environment for all.
Promote quality of life, healthy development and best practices at all stages of life.
This progressive evolution of the Healthy People initiative reflects a growing understanding of the importance of a comprehensive and collaborative approach to national health improvement.
What is Health and Wellness?
Health can be defined in a variety of ways, reflecting its complexity. According to the World Health Organization (WHO), health is “a state of complete physical, mental, and social well-being, not just the absence of disease.” This definition emphasizes that health goes beyond simply being immune to disease and includes a sense of overall well-being. Health is also an individual concept, which means it varies based on individual values, personality, and lifestyle choices. In addition, cultural differences influence how health is perceived and managed, further defining the subjectivity of the concept.
Definition of Health and Wellness
Pender’s definition of health expands on this idea by focusing on self-actualization and the importance of goal-directed behavior. According to Pender, health includes realizing one’s potential through activities such as self-care and maintaining satisfying relationships. It also involves changing one’s environment to maintain harmony, emphasizing the dynamic nature of health as a continuous process rather than a static state
Many factors affect health, and lifestyle plays a major role. Socioeconomic factors such as environment, diet, and lifestyle choices can affect health long before symptoms appear. These factors tend to improve overall well-being or the risk of health problems. Furthermore, personal understanding plays an important role in understanding health and illness. For example, someone with controlled epilepsy may not view their condition as an “illness,” showing that perceptions of health and illness are often subjective and influenced by personal experience and societal views.
The Health and Wellness belief, Health and Wellness promotion, basic human needs, and holistic health models.
Several models offer frameworks for understanding health and illness, each emphasizing unique aspects of human well-being and behavior.
The health belief model developed by Rosenstock, Baker, and Maiman explains how individual beliefs influence health behaviors. It has three components. First, perceived susceptibility reflects a person’s perception of personal risk, such as a family history of heart disease. Second, perceived seriousness includes how seriously a person views health risks, typically influenced by factors such as demographics and external cues, such as news reports or advice from health care from employees and determines it Influence decisions to encourage health-promoting behaviors
Health and Wellness belief model
The Health and Wellness Promotion Model (HPM), proposed by Pender, conceptualizes health as a positive, dynamic state, focusing on well-being rather than merely the absence of disease. This model emphasizes several key areas: the individual characteristics and experiences that influence health behaviors, the knowledge and emotional responses related to specific behaviors, and the Behavioral Outcomes where health-promoting actions result in improved health and quality of life.
Maslow’s hierarchy of needs provides an alternative view of health, proposing a pyramid-like structure of needs. According to this model, basic physical needs such as food, water and safety must be met before higher order needs such as love, esteem and self-awareness In health care, these programs prioritizes needs based on patient’s individual circumstances after surgery while patient emotional Health is addressed
The holistic model of health emphasizes the connection between emotional, spiritual, and physical well-being. This model sees patients as active participants in their health, emphasizing the importance of a comprehensive approach to patient care. Complementary therapies such as meditation, music therapy, touch therapy and guided imagery are central to this model. These interventions are noninvasive, cost-effective, and support natural healing by addressing the whole person and not just physical symptoms.
Health and Wellness promotion for the elderly
Health promotion for older adults focuses on promoting physical activity, personal responsibility, and stress management, as well as increasing social support and community-based programs access to reduce isolation A variety of factors affect older adults’ participation in health services, including their socioeconomic status , personal beliefs; and access to resources is A comprehensive approach to promoting the health of older adults includes considering these various factors to improve their overall well-being and quality of life.
The Variables Influencing Health and Wellness Beliefs and Practices.
There are some internal and external variables that affect health beliefs and practices.
Internal variables
Metabolic variables are endogenous factors that profoundly affect how individuals view health and illness. One such factor is the developmental dimension, which affects an individual’s understanding and coping strategies in relation to health. For example, a child’s diagnosis differs from an adult’s differences in cognitive and emotional development. Nurses must adapt their care and teaching strategies according to the patient’s developmental readiness to ensure effective communication and care.
Another key internal variable is intellectual background, which includes one’s knowledge and intellectual abilities, shaped by education and personal experiences. This factor affects health trust and decision-making, affecting how patients interpret medical information and make health care choices. Nurses must tailor their communication to fit patients in their understanding and present information in a manner consistent with their cognitive abilities.
Performance reflects a person’s perception of their health based on subjective feelings such as fatigue or pain, and objective measurements such as blood pressure Nurses collect subjective and objective information to develop appropriate care plans and realistic goals are set in line with patients’ perspectives and health status.
Emotional Factors also play a significant role in health. Emotional states like stress, fear, or depression can influence how patients react to health issues. For instance, an emotionally resilient person may calmly cope with illness, while someone experiencing high anxiety might avoid addressing symptoms altogether. Nurses must recognize these emotional differences and offer tailored support to help patients navigate their health challenges.
Finally, Spiritual Factors shape an individual’s values and decisions, including health-related choices. Spiritual beliefs may lead some patients to refuse certain treatments, such as blood transfusions in the case of Jehovah’s Witnesses. Nurses must understand and respect these beliefs, integrating them into care to provide holistic, culturally sensitive treatment.
External Variables
External variables include social, family, and cultural factors that affect health behaviors. Family behaviors are exogenous variables, as health behaviors and attitudes toward preventive care, critical illness, and health care interventions are often inherited through family behaviors so Nurses should assess patients’ family health characteristics to better understand possibilities and guide care decisions accordingly.
Psychosocial and socioeconomic factors also play an important role in health outcomes. Social stability, economic status, and support systems can have a profound effect on health. For example, patients facing financial difficulties may prioritize basic living expenses over health care needs, which may affect their ability to adhere to prescribed medications or maintain a healthy diet Nurses need to take those factors into account when designing care plans, and ensuring that practical and realistic solutions are provided in line with patient situations.
Cultural factors are another external variable affecting health. Cultural beliefs influence how individuals understand health, the causes of disease, and treatment preferences. Nurses should avoid stereotyping and instead explore each patient’s unique cultural beliefs. Culturally sensitive care helps nurses communicate effectively and supports patient-centered care by respecting individual practices such as dietary restrictions or the use of traditional resources.
Implications for Patient-Centered Care
In the context of patient-centered care, cultural awareness is crucial. Recognizing that cultural differences affect health perceptions and illness management allows healthcare providers to offer more tailored and respectful care. Cultural beliefs can influence a patient’s willingness to follow a treatment plan or their perception of illness severity, so understanding these differences is key to effective care.
It is also important to avoid stereotyping, as each individual’s health beliefs can vary, even within the same cultural group. Nurses must take the time to understand the specific needs and preferences of each patient, rather than assuming that all individuals from a particular cultural group hold the same views.
Lastly, effective communication is essential for patient-centered care. Utilizing interpreters and culturally appropriate resources, when necessary, ensures that health information is conveyed accurately and is fully understood by patients, supporting informed decision-making and fostering better health outcomes.
The Health and Wellness Promotion, and illness prevention activities.
Today, health care is increasingly focused on health promotion, enhancing well-being, and preventing disease. These actions are necessary to reduce the incidence of disease and disability and overall healthcare costs. By understanding the role of health promotion, wellness, and disease prevention, nurses can better help patients achieve better health.
Key Concepts in Health and Wellness Promotion, Wellness, and Illness Prevention
Health promotion encourages individuals to adopt behaviors that maintain or improve their current health status. This can include regular exercise, healthy eating habits, and other proactive measures. Health promotion aims to motivate individuals to achieve higher and more robust health. It is an ongoing process that encourages individuals to pursue their own interests.
Wellness theory focuses on self-care strategies that contribute to overall well-being. It covers a wide range of topics including body awareness, stress management and personal responsibility. By empowering individuals with knowledge, wellness education enables people to take control of their health and lifestyle, giving them responsibility for their own well-being.
Illness prevention involves specific actions aimed at protecting individuals from potential health risks. For example, immunization programs help prevent the onset of certain diseases, thereby reducing the risk of health decline. Illness prevention is proactive, working to reduce the likelihood of illness and its associated complications.
Together, these concepts create a holistic health approach that goes beyond simply treating illness. They aim to improve well-being across all dimensions of life, not just physical health, thus contributing to a more comprehensive approach to healthcare.
Evidence-Based Health and Wellness Promotion Strategies and Practices
Nurses use a variety of strategies to promote health and encourage patients’ lifestyle changes. These strategies are based on evidence-based practice and are important in supporting patient health goals. Some effective psychosocial strategies are:
Faith Community Nursing (FCN): Members work to promote overall health and wellness in the faith community, meeting physical and spiritual needs. FCN programs typically focus on preventing and promoting social change. Although the outcomes of FCN programs are still being studied, it is recognized that they have the potential to improve health and well-being at the local level.
Motivational interviewing (MI): This face-to-face approach helps nurses understand patients’ motivations and readiness to change. MI strategies aim to reduce resistance to lifestyle change, and empower individuals to manage their health. Research shows that MI is particularly effective in promoting physical activity and supporting behavioral research.
Healthy People 2020 Objectives
The Healthy People 2020 initiative outlines specific health promotion and prevention goals across various areas, which healthcare providers can use to guide their practice. These objectives focus on:
- Physical activity
- Tobacco and substance use
- Sexual health
- Mental health
- Environmental health
- Immunization and infectious diseases
By addressing these objectives, healthcare providers can encourage healthier lifestyles and help prevent illness in diverse populations. The goals set by Healthy People 2020 serve as a benchmark for promoting health and well-being, while also working toward reducing health disparities and improving overall health outcomes.
The Three Levels of Preventive Health and Wellness Care.
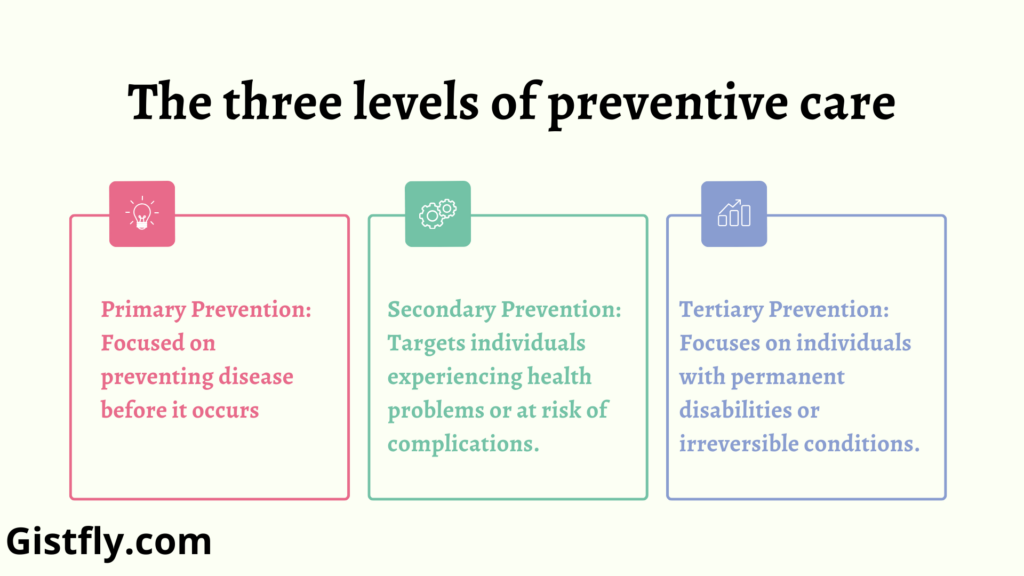
Nursing care for health promotion, wellness, and illness prevention is often divided into three levels: primary, secondary, and tertiary prevention. Each level serves a unique purpose in health care:
- Primary Prevention: Focused on preventing disease before it occurs. This level includes health education, immunizations, and general wellness activities. Primary prevention applies to those in good health, promoting behaviors that help sustain or improve health.
- Secondary Prevention: Targets individuals experiencing health problems or at risk of complications. Early diagnosis and prompt intervention are key, aiming to restore normal health levels and limit disease progression. Secondary prevention includes screenings and treatments that help manage the early stages of illness.
- Tertiary Prevention: Focuses on individuals with permanent disabilities or irreversible conditions. It aims to minimize the effects of chronic diseases through rehabilitation and interventions that prevent further deterioration. For example, a patient with a spinal cord injury may receive physical therapy to maximize their functional abilities and independence.
Four types of risk factors affecting Health and Wellness.
These factors are critical considerations in health promotion and illness prevention, as they provide insight into areas where health risks can be reduced or managed. Nurses and other healthcare providers assess risk factors to guide patients in making informed lifestyle changes that enhance wellness and minimize health threats. The main categories of risk factors include genetic and physiological factors, age, environment, and lifestyle.
Key Categories of Risk Factors
Genetics and physiology
Genetic and physiological factors include physical and functional aspects of the body, which can significantly affect health. Being overweight, for example, puts a lot of strain on circulation, exacerbating cardiovascular problems. In addition, genetic predisposition plays an important role in determining susceptibility to fragile conditions. Individuals with a family history of diseases such as diabetes, cancer, and heart disease are at increased risk of developing these diseases themselves. Understanding these factors enables health care providers to identify individuals who may benefit from strategies prevention or early intervention.
Age
Age is an important risk factor for certain health conditions. For example, babies are more susceptible to diseases due to a developing immune system, while older adults increase the risk of chronic diseases such as heart disease, diabetes, and some cancers are severe, age-related health risks can be reduced through regular screening and screening. Health professionals often recommend screening at specific ages to help identify health problems early, allowing for timely intervention. Routine screening tailored to the person’s age and health history is necessary to minimize the impact of age-related conditions.
Environment
Environment has a profound effect on health. Exposure to air, water, and pollutants can also affect individual well-being. For example, industrial workers exposed to toxic chemicals are more likely to develop respiratory issues or cancer. Nurses and health care professionals assess individual and community environmental risk factors considering the potential short-term and long-term effects of exposure to harmful substances If they hear these environments, understanding these environmental risks enables health care providers to take steps to prevent or reduce environmental exposures by improving overall health outcomes.
Lifestyle
Lifestyle choices play an important role in determining health outcomes. Behaviors such as smoking, poor diet, lack of physical activity, and excessive alcohol consumption are well-established risk factors for various diseases such as heart disease, cancer and diabetes In addition, stress is an important aspect of life that can negatively affect mood and physical health. Prolonged or severe stress can lead to conditions such as heartburn, stomach problems and hot flashes. Nurses play an important role in educating patients about the health risks associated with these behaviors and promoting healthy lifestyle choices. Encouraging positive changes such as quitting smoking, adopting a balanced diet, increasing physical activity and managing stress are important to raise the chances of developing chronic health conditions.
The Role of Nurses in Risk Factor Modification
Risk identification and modification are important components of nursing care, as they help patients understand risk factors and make informed decisions about their health. Nurses play an important role in guiding patients in the process of risk reduction. Below are the main strategies nurses use to help patients reduce health risks:
Risk assessment and health assessment
Nurses often use health risk assessment tools to assess personal risk factors, including lifestyle choices and environmental exposures. These tools provide a systematic approach to identifying areas where patients can improve their health and prevent disease. Assessing the patient’s risk profile can help nurses identify specific behaviors or conditions that require close monitoring, facilitating the development of personalized plans of care.
Education and Mentoring
Educating patients about the health risks associated with behaviors such as poor nutrition or lack of physical activity is an important part of nursing care. Nurses provide information on how healthy choices can positively impact their health. This education can also provide patients with additional resources, such as support groups or community programs, to further assist them in making lasting lifestyle changes
Supporting social change
Nurses help patients set realistic health goals, providing motivation and guidance throughout the process. Strategies such as motivational interviewing can be used to encourage individuals to make basic changes such as quitting smoking or adopting a healthier diet. Nurses help patients provide ongoing support with community resources, such as health care, and promote long-term lifestyle change.
Evaluation and follow-up
Regular monitoring of patient progress is essential to ensure that health goals are achieved and maintained. Nurses help adjust goals as needed and provide follow-up care to ensure long-term sustainability of lifestyle changes. This ongoing support helps patients stay on track, reducing the potential for health issues associated with unadjusted risk factors.
The Importance of Risk Factor Modification
Modifying risk factors is crucial not only for improving individual health but also for reducing overall healthcare costs. By preventing illness through the management of risk factors, the need for extensive medical treatments is reduced, alleviating the financial burden on the healthcare system. For individuals, addressing these risks enhances their quality of life, promotes longevity, and increases their resilience to potential illnesses. By actively involving patients in health promotion efforts, nurses help reduce health disparities and empower individuals to take control of their health, ultimately contributing to healthier communities.
