Nursing Assessment
Nursing assessment is the first and most important step in the nursing process, laying the foundation for effective patient care. This requires more than just data collection; That includes building relationships, using critical thinking skills, and interpreting data to better understand patients’ needs. This section will introduce you to the basic components of a comprehensive nursing assessment, such as the collection of subjective and relevant data, patient-centered interviews, and interpretation of findings. You will learn how interacting with patients through courtesy, comfort, and communication improves the accuracy of your assessment, and how this process leads to informed medical decisions and patient care planning Let’s go deeper into the essentials a it validates the quality of nursing research.
By the end of this section, you should know about:
- The relationship between critical thinking and nursing assessment.
- How developing relationships with patients fosters the assessment process.
- How courtesy, comfort, connection, and confirmation establish a foundation for patient assessment.
- The difference between subjective and objective data.
- The ways to make an assessment patient centered.
- The methods of data collection.
- How to conduct a patient-centered interview.
- The components of nursing history.
- The relationship between data interpretation and validation.
- Conduct a nursing assessment.
Let’s take a closer look at them.
Test Your Knowledge
At the end of this section, take a fast and free pop quiz to see how much you know about Nursing Assessment.
The relationship between critical thinking and nursing assessment.
Critical thinking is foundational to the nursing assessment process, as it enables nurses to approach patient care systematically and holistically. It involves collecting, interpreting, and analyzing data using clinical skills and logical reasoning. For example, when a nurse notices a patient hallucinating, they do not simply record a diagnosis but suggest possible causes such as pain or discomfort based on knowledge of the patient’s medical history and current condition. This rigorous thinking allows for accurate nursing assessment and effective care planning.
How developing relationships with patients fosters the nursing assessment process.
Establishing a trusting relationship with patients is essential to a quality assessment. This relationship creates an environment where patients feel comfortable sharing sensitive or personal information, which can be critical to their care. When nurses engage in meaningful communication and show empathy, patients are more open about their concerns, such as fears of diagnosis or challenges in managing their health It also provides depth improve, and ultimately enhance, care outcomes.
How courtesy, comfort, connection, and confirmation establish a foundation for patient nursing assessment.
Courtesy, comfort, connection, and confirmation are principles that guide effective nursing assessments. Courtesy involves introducing oneself respectfully, addressing the patient by their preferred name, and explaining the purpose of the interaction to maintain transparency. Comfort focuses on ensuring that the environment is conducive to open dialogue, such as providing privacy and addressing pain or fatigue before beginning the assessment. Connection is about building rapport through active listening, empathy, and meaningful eye contact to foster trust. Lastly, confirmation ensures the accuracy of the collected information by summarizing key points and asking the patient to validate the findings. These principles collectively create a supportive atmosphere where patients feel valued and understood.
Courtesy: Address the patient by their preferred name, introduce yourself, and explain your role. Ensure that all information will be kept confidential and follow HIPAA guidelines.
Comfort: Ensure the environment is comfortable and conducive to an effective interview. Address the patient’s comfort needs (such as pain or fatigue) and maintain privacy.
Connection: Create a positive first impression, make eye contact, and engage actively with the patient. Start with open-ended questions to encourage patients to share their concerns.
Confirmation: At the end of the interview, ask the patient to summarize the discussion and clarify any uncertainties. This ensures all concerns are addressed.
The difference between subjective and objective data in nursing assessment
Subjective data refers to information shared by the patient about their feelings, experiences, and perceptions. This includes descriptions of pain, nausea, or emotional states like anxiety. For instance, a patient saying, “I feel sharp pain in my abdomen,” is providing subjective data. Objective data, on the other hand, is measurable and observable, such as vital signs, lab results, or physical examination findings. A nurse documenting a patient’s temperature as 101°F or nothing redness and swelling around a wound is recording objective data. Together, these data types form the basis for understanding the patient’s condition comprehensively and guide clinical decision-making.
The ways to make an assessment patient centered in nursing assessment
A patient-centered assessment emphasizes collaboration and respect for the patient’s unique experiences, preferences, and needs. Nurses should actively involve the patient in the assessment process by asking open-ended questions, using clear and empathetic communication, and considering the patient’s cultural background and personal values. For example, a nurse might ask, “Can you describe how your symptoms affect your daily life?” This approach encourages patients to share their perspectives, ensuring the assessment reflects their specific challenges and goals. Patient-centered care promotes mutual respect and enhances the quality of the assessment by addressing physical, emotional, and psychosocial aspects of health.
The methods of data collection in nursing assessment
Nurses gather data through multiple methods, including interviews, physical examinations, and reviewing medical records. The patient is often the primary source of information, but family members, other healthcare providers, and diagnostic tests can provide additional insights. Observing nonverbal cues, such as facial expressions or body language, can reveal pain or discomfort that a patient might not verbalize. Tools like questionnaires or health literacy assessments can further support data collection. For instance, using a tool like PQRST (Provokes, Quality, Radiates, Severity, Time) helps organize information about a patient’s symptoms systematically, ensuring that no critical details are overlooked.
How to conduct a patient-centered interview in nursing assessment
The patient-centered interview is a structured yet relational method designed to build trust, build partnerships, and gather information about patients while promoting a collaborative care environment It aims to gather comprehensive data, understand patient concerns, and establish the therapeutic relationship as a basis for effective care. This process combines several basic principles. Motivational interviewing helps manage a patient’s ambivalence about change, allowing them to clear uncertainty and make informed decisions about medical or lifestyle changes. Effective communication skills play an important role, with courtesy, comfort, communication and empowerment being important factors. Nurses should communicate respectfully with patients, ensure confidentiality, create a comfortable and private environment, build rapport through active listening and eye contact, and emphasize key points at the end of the communication to clarify any uncertainties.
Preparation is essential for a successful interview. By reviewing the patient’s medical record first, he or she can ask appropriate follow-up questions and tailor the conversation. The interview usually consists of three parts. During the orientation phase, the nurse introduces herself, explains the reason for the interview, and sets the agenda by encouraging the client to discuss her concerns. Finally, the closing phase allows the nurse to summarize the data collected, verify its accuracy, and address any remaining questions or concerns.
Strategies to conduct a patient-centered interview
Several strategies improve patient-focused interviews. Guiding the conversation ensures that the conversation remains focused and allows the patient to share their story. Interviews can be focused, covering specific topics such as follow-up, or more comprehensive, covering all aspects of the patient’s history. Subjective information such as reports of symptoms verified by objective data from physical examination or diagnostic tests ensures accuracy and reliability e.g., as a patient reports difficulty breathing, the nurse should confirm this by assessing vital signs and bronchoscopy.
In practice, Mr. Lawson’s model illustrates the stages of a patient-centered interview. During the orientation, the nurse introduces herself, explains her role, and explains why she was interviewed. Open-ended questions in the administrative section allow Mr. Lawson to discuss his concerns about the management of his health after discharge. The closing stage wraps up the conversation and ensures she feels confident in the next step.
Observations play an important role in patient-focused interviews, as verbal communication is often supported by nonverbal cues. Eye contact, body language, tone of voice, and general appearance reveal a patient’s emotional state, discomfort, or self-care ability. Comparing nonverbal cues with verbal information helps the nurse assess consistency and accuracy.
Types of Questions in a Patient-Centered Interview
Different questions serve different purposes in an interview. Open-ended questions encourage patients to elaborate on their thoughts and feelings, whereas leading questions, although less positive, can influence responses. Back channeling, such as using language cues like “uh-huh” or “go on,” reinforces active listening and encourages patients to expand. Probing questions delve into specific concerns, direct closed questions clarify specific issues with short answers such as frequency or severity of symptoms
Conducting a thorough and accurate interview requires careful observation, clear communication, and acknowledgment of ambiguity. Nurses ensure that the patient’s story is well heard, synthesizing contextual information and objective findings to develop a clear understanding of the patient’s health Key Practices Start with open-ended questions, watch for signs that aren’t verbally, use surveys and follow-up techniques to engage the patient, and use closed-ended questions when specific information is needed include avoiding assumptions and Acknowledgment and clarification of ambiguities is essential to ensure accuracy in nursing diagnosis and care planning. This comprehensive approach ensures that the patient receives appropriate and effective care.
The components of nursing history.
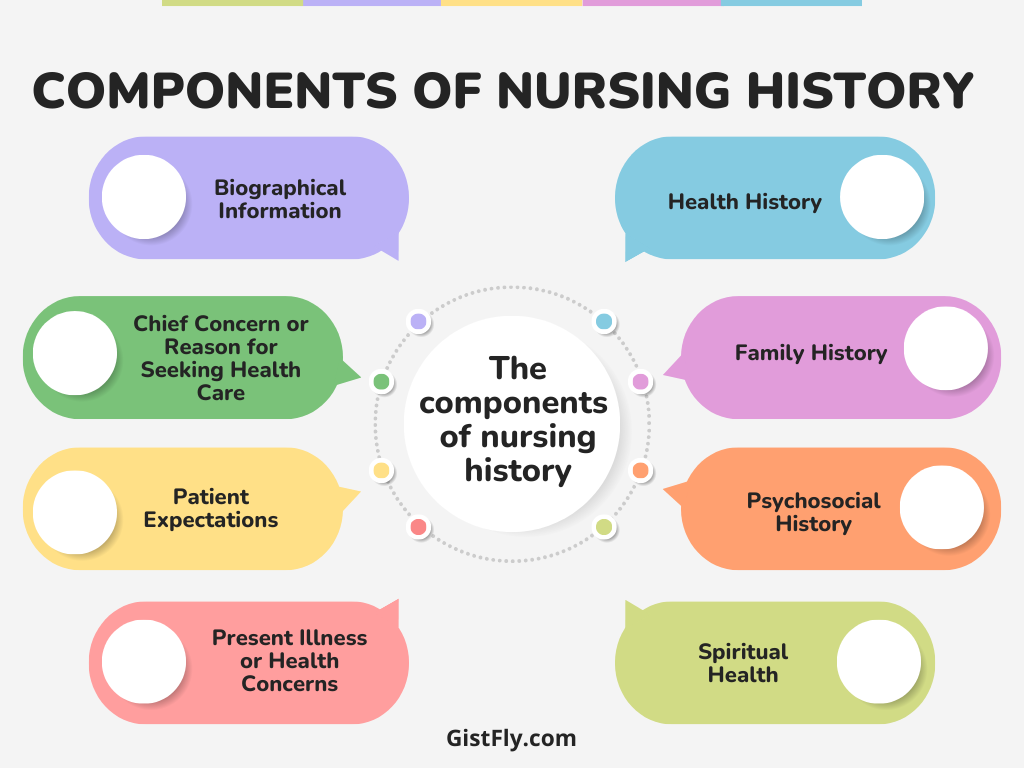
A comprehensive nursing history includes several key components:
Biographical Information:
This includes basic demographic information, such as age, address, occupation, marital status, and source of health care. Typically, this data is collected by the admitting staff.
Chief Concern or Reason for Seeking Health Care:
This is the patient’s primary reason for seeking care. The nurse should ask open-ended questions to understand the patient’s concerns, which are recorded as subjective data. This can reveal more than just the chief complaint on the admission sheet.
Patient Expectations:
A nurse should assess the patient’s expectations, which may include desires for diagnosis, symptom relief, comfort measures, and successful treatment. Meeting these expectations is key to patient satisfaction.
Present Illness or Health Concerns:
Using the PQRST acronym (Provokes, Quality, Radiates, Severity, Time), the nurse gathers detailed information about the patient’s symptoms, their onset, duration, triggers, and intensity.
Health History:
A thorough history includes previous hospitalizations, surgeries, and illnesses. Medication history, including prescriptions, OTC drugs, and herbal remedies, is also crucial. Allergies and reactions to substances like food or latex are important to note.
Family History:
This provides insights into genetic or familial risks for certain health conditions, helping to identify areas for health promotion and prevention.
Psychosocial History:
This includes information about the patient’s support system, coping mechanisms, and any stress or recent losses. It helps identify potential areas for psychological or social interventions.
Spiritual Health:
The nurse should assess the patient’s spiritual beliefs and practices, which may be significant in their overall health care. This can also include rituals and the patient’s relationship with faith, especially in a healthcare setting.
Review of Systems (ROS):
The ROS is a comprehensive review of all body systems to identify any symptoms or changes. This includes questions about the skin, cardiovascular system, respiratory system, etc.
Together, these components provide a holistic view of the patient’s health and guide personalized care planning.
The relationship between data interpretation and validation.
Data interpretation involves analyzing the collected data to identify patterns or trends indicative of specific health issues. For example, a cluster of symptoms such as fever, rash, and oozing wound may indicate the presence of infection. Validation ensures the accuracy of these definitions by cross-specing with other sources such as the patient, family members, or medical records. For example, if a patient complains of chest pain, the nurse can verify this by performing and reviewing physical examination diagnostic tests. Accurate interpretation and validation is essential for reliable nursing assessment and prevention of errors.
Interpreting Assessment Data
Interpretation: The nurse uses clinical reasoning to identify patterns in the data collected and recognize the presence of abnormal findings. Validating the data helps ensure completeness and accuracy.
Data Clusters: A nurse groups signs and symptoms into logical clusters that begin to reveal the patient’s health problems. This helps guide the next steps in planning care.
In nursing practice, data clusters play an essential role in clinical decision-making and identifying patient problems. By organizing collected assessment data into clusters, nurses can discern patterns that help in forming a comprehensive understanding of the patient’s condition. The ability to recognize and interpret these clusters is critical to making accurate diagnoses and planning effective interventions. The data set is a group of related signs, symptoms, or behaviors that, when analyzed together, provide valuable insight into a patient’s health status Once someone gets out of bed, etc. It reveals more. Behavioral symptoms such as anxiety, poor eye contact, restlessness, and constant questioning indicate a high level of distress or anxiety.
Additionally, knowledge and educational needs are evident as the patient asks more questions about postoperative care and expresses concerns about surgical incisions, risk of infection, and dressing appearance These findings indicate the need for detailed explanations about self-care and competency expectations. Considered together, these groups depict a multifaceted narrative including postoperative pain and uncertainty, potential risks of infection, and differences in understanding of postoperative care.
Validating Assessment Data
Once data clusters are recognized, it is crucial to validate them to ensure accuracy and prevent misinterpretation. For instance, while a nurse might infer that a patient’s tears are related to their hospitalization, it is important to ask the patient directly to confirm the cause: “I notice you’ve been crying; can you tell me more about how you’re feeling?”
Validating data may also involve cross-checking with other sources, such as family members, medical records, or the rest of the health care team. This process ensures that the data gathered is correct and comprehensive, which is essential for forming an accurate clinical picture.
Critical thinking and reflection are integral to data interpretation and care planning. For example, Tonya’s assessment of Mr. Lawson’s health involves identifying patterns in his discomfort and anxiety post-surgery, leading her to prioritize interventions to manage pain, reduce infection risk, and address his education needs.
Using concept mapping is an effective method for organizing and connecting these findings. Concept maps help nurses visualize relationships among different health problems, promoting a holistic understanding of the patient’s needs. Tonya’s concept map for Mr. Lawson helps her see the interconnections between his pain, risk of infection, and educational needs, leading to targeted nursing interventions.
Data Documentation
Accurate and timely documentation is essential for continuity of care and for communicating findings across the healthcare team. All observations, both subjective and objective, should be recorded clearly and concisely. For example, subjective data should be written in quotation marks to reflect the patient’s own words, while objective findings should be documented using precise measurements (e.g., “weight: 77.2 kg, abdomen soft and nontender”).
By documenting thoroughly, nurses ensure that essential information is available for follow-up assessments, interventions, and evaluations, helping to ensure optimal patient outcomes.
Conduct a nursing assessment.
Conducting a nursing assessment involves collecting subjective and objective data through interviews, observations, and physical examinations. The nurse uses open-ended questions to assess the patient’s concerns, observe for nonverbal cues, and thoroughly assess normal body systems such as monitoring the surgical wound for redness or eczema swelling, palpating for tenderness, and measuring vital signs are key factors. The information is then systematically recorded, and the findings are communicated to the health care team to guide the next steps in care. The ongoing nature of research ensures that emerging patient needs are met promptly, leading to optimal outcomes.
