Older Adults
Older adults need care and in order to properly do that one should understand the common myths and physiological changes of aging. Key concerns include managing chronic conditions, mental health issues like depression and dementia, and supporting social engagement. Nurses play a vital role in addressing both cognitive and psychosocial challenges, ensuring older adults maintain independence and quality of life.
By the end of this section, you should know about:
- The common myths and stereotypes about older adults.
- The common developmental tasks of older adults.
- The common physiological changes of aging.
- Delirium, Dementia, and Depression.
- The issues related to psychosocial changes of aging.
- The multifaceted aspects of elder mistreatment.
- Selected health concerns of older adults.
- Nursing interventions related to the physiological, cognitive, and psychosocial changes of aging.
Let’s take a closer look at them.
Test Your Knowledge
At the end of this section, take a fast and free pop quiz to see how much you know about Older Adults.
The common myths and stereotypes about older adults.
There is the Negative Perceptions. Misconceptions about aging persist, including stereotypes that older adults are sickly, disabled, and unattractive, or that they are forgetful, unproductive, and unable to learn. Such beliefs are not only inaccurate but can lead healthcare providers to deliver lower-quality care. Also, there are some positive attributes overlooked. In reality, older adults often have an optimistic outlook, retain good memories, maintain social connections, and continue to learn throughout their lives. Physical changes, like reduced energy or changes in hearing and vision, may affect learning, but they are far from barriers to continued growth.
Many believe older adults face financial challenges or are affluent, but the truth is more nuanced. In 2014, 9.5% of those over 65 were below the poverty line, with poverty rates higher among older women (11.6%) than men (6.8%). Moreover, ageism is discrimination based on age, undervaluing older people and often equating worth with youth and productivity. This bias can erode self-confidence in older adults, limit their access to care, and mislead caregivers. Nurses have a duty to counteract ageism by promoting positive views of aging and respecting the individuality of each older adult.
Contributions and Social Role of Older Adults
Older adults have a strong economic presence and political power as active consumers and voters. Their contributions to public policy and community affairs are significant, as they represent a large, experienced demographic with unique perspectives on various issues. Moreover, older adults have lived through major historical and technological shifts—from the Great Depression and two World Wars to recent conflicts and advancements in technology. They witnessed transformations in healthcare, from general family physicians to specialized medical fields, and have observed the development of key social programs like Social Security, Medicare, and Medicaid. Adapting to Change. Having seen extensive societal and healthcare changes, older adults have valuable insights on resilience and adaptation that can be shared with younger generations. Their life stories reflect decades of coping strategies and offer lessons on how to navigate change and uncertainty.
Ageism: Ageism refers to the discrimination or stereotyping of individuals based on their age, particularly towards older adults. It involves negative attitudes, biases, and assumptions about the abilities, worth, or value of older individuals.
The common developmental tasks of older adults.
Social development: Developmental work in adulthood focuses on adapting to physical, social, and emotional changes. Although developmental stages vary from person to person, researchers have identified common developmental functions in older adults. These tasks may involve coping with loss of health, relationships, social activities, income and independence. Older adults are often challenged to adjust to declining health and physical fitness, cope with retirement, reduced or fixed income, lack loved ones such as a spouse, siblings, or friends’ death, and do not recognize themselves as older individuals who are redefining and maintaining a good life through various means
Making Physical Changes: Physical growth varies from person to person and does not necessarily indicate illness. However, changes in the appearance and function of our skin are common. Some individuals find it difficult to accept aging, often underestimating their age, dressing younger, or using cosmetics to hide signs of aging Others may encounter decline in activity, and avoiding seeking help for certain projects may jeopardize their safety. Retirement and Role Adjustments: Retirement often involves adjusting to a loss of work identity. Some retirees view it as an opportunity to pursue new interests, engage in community service, or continue learning. Others might change their living arrangements due to physical limitations, moving to smaller homes or care facilities. This process requires a period of adjustment and support from family and healthcare professionals.
More developmental tasks of older adults
Coping with Loss and Grief: Many older adults experience the death of a spouse; as of 2013, 36% of older women were widows and 12% of older men were widowers. Some may also face the loss of adult children, grandchildren, or friends, which not only brings sorrow but serves as a reminder of their own mortality. Nurses can support older adults through grief by helping them process loss and accept the emotional impact of these changes.
Evolving Family Dynamics: Relationships with adult children continue to evolve as older adults age, bringing new challenges around decision-making, dependency, and sometimes conflict or guilt. When adult children assume caregiving roles, they may struggle to balance these responsibilities with their own family and career demands. Nurses can play a valuable role by counseling families, helping them navigate complex emotional dynamics, and maintaining quality of life for older adults.
Quality of Life: Maintaining a high quality of life is a priority for older adults, and the definition of “quality” is unique for each person. This can involve fulfilling personal interests, enjoying meaningful relationships, or staying connected to the community.
The common physiological changes of aging for older adults.
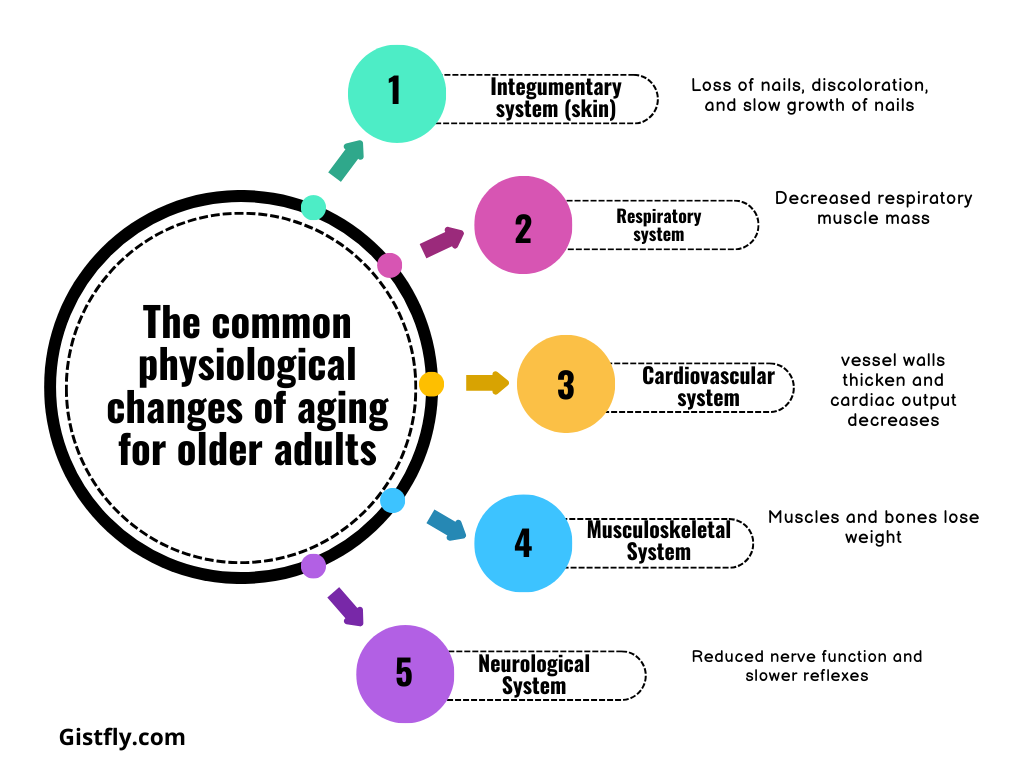
Integumentary system (skin): loss of nails, discoloration, and slow growth of nails. Check regularly for skin lesions or growths that may require further evaluation.
Respiratory system: Decreased respiratory muscle mass and muscle mass make older adults more susceptible to respiratory diseases; Check for signs of pneumonia.
Cardiovascular system: vessel walls thicken and cardiac output decreases; Promotes cardiovascular health by controlling blood pressure.
Gastrointestinal system: prolonged peristalsis and decreased content of food. This can lead to constipation, so be sure to eat fiber and water.
Musculoskeletal System: Muscles and bones lose weight, so encourage regular exercise to stay strong and mobile.
Neurological System: Reduced nerve function and slower reflexes. Address sleep concerns through environmental modifications and a regular sleep schedule.
Delirium, Dementia, and Depression for older adults.
Dementia, Delirium, and Depression are conditions that affect cognition in older adults, often presenting similarly but with important distinctions in onset, progression, duration, and associated features.
Delirium: This condition typically has a sudden onset, fluctuates daily (often worse at night or in low-light conditions), and is usually short-lived. Delirium is often caused by acute physiological issues such as electrolyte imbalances, infection, or medication effects. It’s marked by impaired consciousness and fluctuating alertness, with patients frequently experiencing disorientation and fragmented thinking, sometimes with hallucinations. Due to its reversible nature, timely intervention based on a thorough assessment of the underlying cause is crucial.
Dementia: Unlike delirium, dementia is a gradual and progressive decline in cognitive function that is irreversible. The most common forms include Alzheimer’s disease and vascular dementia, which impair the ability to perform daily activities over months or years. Patients with dementia may struggle with memory, especially recent memories, and may have difficulty with abstract thinking and judgment. Their awareness is usually intact, although they may attempt to hide cognitive deficits. Nursing care for dementia focuses on safety, enhancing quality of life, and adapting support to the individual’s evolving needs.
Depression: Depression often coexists with other cognitive conditions and can be mistaken for dementia. It may have a gradual or abrupt onset, often tied to significant life changes, with symptoms typically worse in the morning. Patients with depression are generally alert and oriented but may show selective disorientation and “patchy” memory. Thought processes are generally intact, though they may center around feelings of hopelessness or helplessness. Depression in older adults requires sensitive assessment, as symptoms can be misinterpreted as dementia, and treating depression can improve quality of life significantly.
Delirium: Delirium is an acute, often reversible condition characterized by a sudden onset of confusion, disorientation, and cognitive disturbances, usually caused by factors like medication, infection, dehydration, or changes in the environment. It commonly affects older adults, particularly in hospital settings, and can result from surgery, medications, or underlying health issues.
Dementia: Dementia is a chronic, progressive decline in cognitive function, which affects memory, thinking, reasoning, and the ability to perform everyday activities. Unlike delirium, which is often reversible, dementia is usually irreversible and is commonly associated with conditions like Alzheimer’s disease.
Depression: Depression is a mood disorder that causes persistent feelings of sadness, hopelessness, and loss of interest or pleasure in daily activities. It can affect older adults due to various factors like isolation, health problems, or life changes, and can often be overlooked in this population.
The issues related to psychosocial changes of aging.
Life transitions and losses: Changes such as retirement, declining health, or the death of a spouse affect older adults the most.
Self-reflection: Encourage discussion about self-identity, relationships, and coping strategies.
Areas of concern: Look at family dynamics, social isolation, housing, health, and spiritual needs.
The multifaceted aspects of elder mistreatment.
Elder mistreatment includes physical abuse, emotional abuse, financial exploitation, neglect, sexual abuse, and abandonment. It is a serious concern, with an estimated 10% of older adults experiencing some form of mistreatment. Moreover, nurses need to be vigilant in screening for signs of abuse, as vulnerable elders may experience a combination of mistreatment types.
Elder mistreatment includes neglecting basic needs such as food, water, shelter, personal hygiene, and medication. Perpetrators of elder abuse are often family members, particularly caregivers. Challenges in identifying abuse arise due to fear of reporting, isolation, and denial. Vulnerable elders may be reluctant to seek help due to fear of retribution or being placed in a nursing home. Programs like the National Center for Elder Abuse (NCEA) and the Elder Justice Act aim to provide resources and funding to combat elder mistreatment, particularly through Adult Protective Services (APS).
Elder mistreatment: Elder mistreatment refers to the abuse, neglect, or exploitation of older adults, either by family members, caregivers, or others in positions of trust. It can include physical, emotional, or financial abuse, as well as neglect or abandonment.
Selected health concerns of older adults.
Older adults often face a variety of health challenges that require targeted interventions and preventive measures. Chronic diseases such as heart disease, hypertension, cancer, COPD, and diabetes are common in this population. Management of these conditions includes lifestyle changes, medication adherence, and symptom management. Functional limitations, including problems with mobility, self-care, and independent living, are also increasing, affecting overall well-being. Mental health problems such as depression, schizophrenia, psychosis are important issues that can lead to social isolation and reduced quality of life. Good nutrition is important for the elderly but times many are hindered by factors such as limited mobility, financial constraints and dental problems. It also remains important for improved cognition, as substance use, including smoking, alcohol, and prescription drug abuse, poses additional health risks that require education and delivery they are involved.
Preventive Health Measures
Preventive health programs play an important role in supporting older adults. Routine check-ups, such as blood pressure screenings, eye exams, and cancer screenings, as well as immunizations such as influenza and pneumonia vaccines, are important to build lifestyle resources emphasize interventions, including healthy eating, regular exercise and stress management. Programs that promote smoking cessation and moderate alcohol consumption help reduce risks associated with chronic diseases.
Teaching Strategies for Older Adults with Health Literacy Limitations
Effective education of older adults requires specific strategies tailored to their needs. Understanding can be enhanced by doing it for short periods of time at high-energy times, using simple language, introducing concepts gradually and varying learning sessions Health concepts are achievable to communicate more by linking new information to previous experiences through storytelling. Family involvement provides additional support and reinforces health issues. Follow-up teaching methods, in which patients repeat instructions, ensure understanding and compliance. Emphasizing issues directly related to everyday life and focusing on practicality and relevance helps improve understanding and accessibility by breaking down instructions into clear and achievable steps deal with the solution.
Health Promotion and Maintenance Interventions
Promoting cardiovascular health involves dietary changes, regular monitoring, and adherence to prescribed medications to manage heart disease and hypertension. Cancer prevention strategies include education on self-examinations, screening tests, and attentiveness to subtle signs of cancer. For respiratory health, smoking cessation and respiratory exercises are particularly important for COPD management. Nutrition counseling, in collaboration with dietitians, helps create accessible and nutrient-rich meal plans, and meal delivery services can be considered when needed. Exercise programs should be individualized, focusing on low-impact activities like walking or swimming and incorporating activities of daily living for those with limited mobility. Mental health support involves early identification of depression or substance abuse, providing counseling resources, and engaging patients in meaningful activities.
Falls in Older Adults
Falls represent a significant safety issue for older adults, often leading to injuries such as fractures in the spine, hip, forearm, and pelvis. Fear of falling after an incident can reduce mobility and physical fitness. Intrinsic risk factors include vision impairment and mobility conditions, while extrinsic factors involve environmental hazards and improper footwear. Prevention strategies, detailed in Chapter 39, are essential to reducing fall risks.
Sensory Impairments
Sensory impairments, including poor vision and hearing, are common among older adults. Supporting sensory function involves the use of assistive devices such as hearing aids and glasses to ensure full engagement in care activities.
Pain Management
Pain is common but not a normal part of growing up. Chronic pain can lead to depression, limited mobility, and withdrawal. Effective pain management is especially important when considering cultural factors, fears about medications, and the challenges of assessing pain in individuals with cognitive impairment.
Medication Use and Polypharmacy
Older adults are more likely to take multiple medications, increasing the risk of drug addiction due to changes in metabolism and interactions. Polypharmacology, or the use of multiple drugs, can lead to inactivation, loss of efficacy, and crashes. Nurses play an important role in medication adherence by providing education and collaborating with health care providers.
Therapeutic Communication
Effective communication with older adults requires both verbal and nonverbal skills, including eye contact, active listening, and empathy. Therapeutic communication helps meet expressed and unexpressed needs and fosters a relationship of respect and caring.
Touch
Touch is an important therapeutic tool for comforting older adults, reducing anxiety, and providing emotional support. Gentle touch promotes relaxation and physical comfort but must consider cultural and individual preferences to avoid being perceived as condescending.
Reality Orientation
Reality orientation is useful for older adults experiencing confusion or disorientation due to illness, surgery, or environmental changes. This technique involves frequent reminders of time, place, and people, supported by environmental aids like clocks and calendars, to reduce confusion and promote stability.
Validation Therapy
Validation therapy is particularly effective for older adults with dementia who are confused or disoriented. Unlike reality orientation, it accepts the individual’s perception of time and place, emphasizing understanding and acknowledging the feelings behind their behavior rather than correcting them. This approach reduces anxiety and builds trust.
Reminiscence
Reminiscence, the process of recalling past experiences, offers emotional and cognitive benefits for older adults. It helps them reflect on achievements, cope with challenges, and resolve unresolved conflicts, boosting self-esteem and providing new meaning to past events. Nurses can use reminiscence as an assessment tool to gauge self-esteem, cognitive function, and emotional stability. It is also used in group therapy for individuals with cognitive impairments or depression, with activities tailored to the group’s needs and goals.
Body-Image Interventions
Body image concerns often arise due to physical effects of aging or illness. While some changes, such as gray hair, are socially accepted, others, like wrinkles or the use of medical devices, may negatively impact self-perception. Chronic illnesses that result in physical dependence can further affect body image. Nurses can assist older adults in maintaining a positive body image by supporting grooming, hygiene, and appearance. Tasks such as hair grooming, denture cleaning, or assisting with dressing can significantly improve self-esteem. Additionally, managing environmental factors such as unpleasant odors from medical conditions helps create a more comfortable atmosphere and encourages social interactions.
Gerontological nursing: is the specialized field of nursing that focuses on the care of older adults. It involves assessing, diagnosing, and treating health issues specific to older individuals, while also addressing their psychological, emotional, and social needs.
Reminiscence: refers to the process of recalling and reflecting on past experiences, particularly positive memories, to bring meaning and understanding to the present. It is often used in older adults to improve self-esteem, emotional well-being, and cognitive function, as well as to resolve unresolved conflicts and reinforce personal identity.
Validation therapy: is a therapeutic technique used with older adults, particularly those with dementia or cognitive impairments, where their feelings, thoughts, and memories are acknowledged and validated. The goal is to reduce distress and improve emotional well-being by accepting the person’s reality, even if it differs from the actual situation.
<strong>Nursing interventions </strong><strong>related to the physiological, cognitive, and psychosocial changes of aging</strong>.
Physiological; Monitor vital signs, encourage mobility, ensure proper nutrition and hydration, manage chronic conditions. Cognitive; Implement reality orientation, provide cognitive stimulation, encourage social interactions. Psychosocial; Offer emotional support, provide opportunities for socialization, assist with decision-making, involve family members in care planning
Older adults in intensive care units face unique challenges and risks that require special attention and care. A major concern is the risk of dementia, which is common in hospitalized older adults and is triggered by a variety of medical and non-medical factors. Medical causes and immobility, insomnia, infection, dehydration, medications, and anesthesia. Non-medical factors may include unfamiliar surroundings, new employees, stress, sensory problems such as vision or hearing loss, and separation from known family members. Factors prevention to manage depression. Reorient the patient with memory cues such as clocks and calendars etc. Reality-orientation techniques can help to condition a person soothe, encourage family visits, and treat the root causes of depression
Dehydration and malnutrition are serious risk factors for older adults during hospitalization. These cases are often the result of diagnostic procedures that already restrict food and fluid intake, as well as medications that reduce appetite or alter food intake. Adding your favorite foods to your meal plan can also stimulate your appetite. It is important to ensure that patients have easy access to food and water, especially if they are bedridden or connected to medical equipment.
More on Nursing interventions
Healthcare-associated infections (HAIs) pose additional risks due to weakened immune systems and underlying chronic conditions in older adults. Common infections include urinary tract infections (UTIs) commonly involving urinary tract infections, and surgical site infections, hematologic infections, and pneumonia Materials prevention Maintain hand hygiene, control infection Attention is also paid following proper isolation procedures.
Urinary incontinence, especially transient urinary incontinence, is common in elderly hospitalized patients. This condition can be caused by trauma, untreated infection, medication, or limited mobility. Interventions for defecation incontinence include providing opportunities for regular defecation and changing the environment to facilitate access to the toilet. To avoid the use of implants to prevent skin breakdown, it is also important to use skin care techniques.
Older adults are at increased risk for pressure sores and skin tears due to changes in skin integrity, lack of mobility, incontinence, and poor nutrition. Preventive measures the mouth includes proper placement, use of supportive materials to relieve pressure, careful skin care, hydration, and ensuring adequate nutrition for supports skin health.
