Professional Nursing
Nursing is a dynamic and evolving profession that responds to the ever-changing health care needs of the public. These needs are determined by different economic, social and cultural factors at different times. As society changes, such as technological advances, changing demographics, growing consumerism, and advocacy groups for health promotion, women’s rights, and human rights, the nursing practice also evolves to meet new demands address this professional nursing definitions, standards, and professional nursing organizations, nursing role, research, and play a key role in guiding education, ensuring it is relevant to today’s healthcare challenges and, as nurses become more politically engaged, strengthening, empowering their ability to influence healthcare policy and practice reinforcing their central role in shaping the future of healthcare.
By the end of this section, you should be able to know about the:
- Development of professional nursing roles.
- Educational programs available for professional registered nurse (RN) education.
- Roles and career opportunities for nurses.
- Influence of social, historical, political, and economic changes on nursing practices.
Let’s take a closer look at them.
Test Your Knowledge
At the end of this section, take a fast and free pop quiz to see how much you know about Professional Nursing : Roles, Education, and Evolving Practices.
Development of professional nursing roles.

Nursing offers career paths including clinical practice, education, research, management, administration, and employment. Nursing means practicing professionally to provide quality patient-centered care in a safe, prudent, and knowledgeable manner. You are responsible and accountable to yourself, your patients, and your peers. Understanding the scope of nursing is important, as it determines how nurses impact patients, families, and communities. Nursing is more than just technology. Nurses are responsible for providing safe and appropriate care, and are accountable to themselves, patients, and peers. This professional approach differentiates nursing as a profession.
Advocacy groups, such as the Robert Wood Johnson Foundation (RWJF) and Future Nursing: Campaign Action, emphasize the role of nursing in transforming health care. This campaign and the Institute of Medicine’s report on the future of nursing focuses on preparing a professional workforce to meet the needs of health promotion, disease prevention and complex care in a rapidly changing health care landscape.
The science and art of nursing practice
By combining nursing scientific expertise with artistic, compassionate care, as patients’ needs diversify and constantly change, nurses must deliver high quality care that incorporates current knowledge, evidence-based practices, and societal standards types mix, and professional partnerships also for Even be involved Use knowledge fully and gain knowledge.
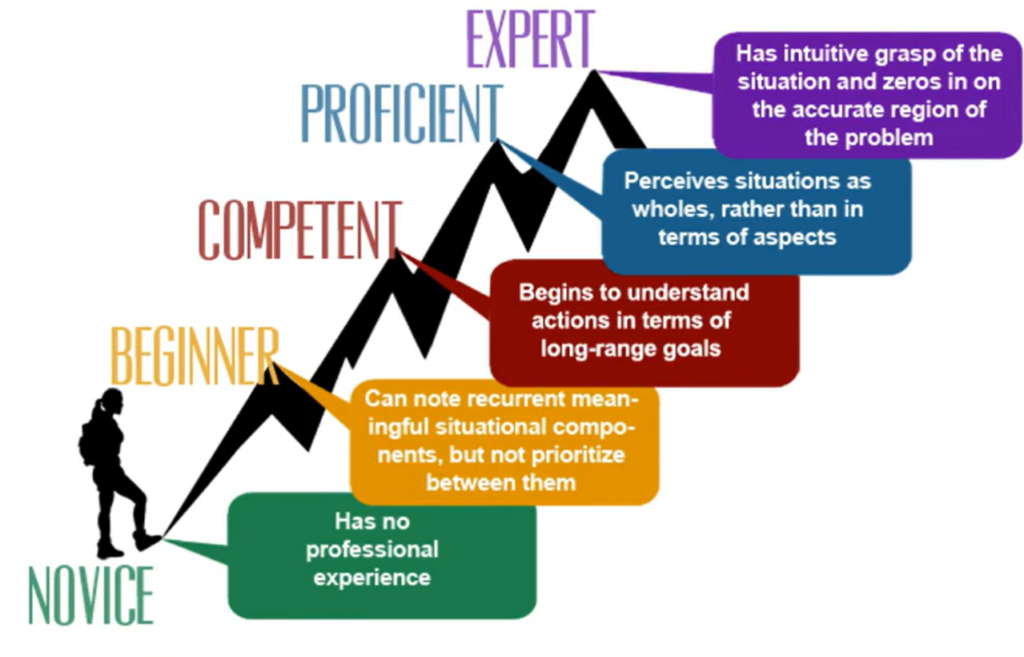
Benner Stages: from novice to expert
According to Patricia Benner (1984), nurses develop through five sets of competencies, acquiring knowledge over time:
Novice: Beginners who follow established rules, and learn in a linear, systematic way.
Beginner: Nurses with some experience can recognize important aspects of care.
Competent: After 2-3 years in the program, nurses understand patient care and are able to set long-term goals.
Proficient: With more than three years of experience, nurses assess situations comprehensively and manage care effectively.
Expert: Experienced nurses readily understand clinical problems and are able to manage complex issues based on patient charts. Those usually have a registered nurse professional license
Critical thinking and clinical decision making
Critical thinking is important in nursing, because it supports interpretation of situations and complex decision-making. Nurses put things together:
Scientific knowledge and experience from basic science and nursing
Prehospital stress conditions
Attitudinal and professional standards, ensuring that each patient receives comprehensive, compassionate care.
Scope and Standards of the Professional Nursing
Nursing care follows standards of practice and codes of ethics defined by the American Nurses Association (ANA) and the International Council of Nurses (ICN), where the ANA defines nursing as health promotion, disease prevention, cessation of suffering, patient advocacy in individual and community care, and the ICN definition states that in nursing All ages as well includes independent and collaborative care Groups and settings, focusing on health promotion, disease prevention, care of the frail, disabled and dying, with other activities including research, health care and education.
ANA’s Scope and Standards of Practice
Since 1960, the ANA has established the scope and standards of nursing practice, which help guide nurses in making significant, visible contributions to patient health and community well-being, while encouraging nurses to know and apply these standards, which are often provided by schools of nursing and practice settings to ensure consistent, quality care.
ANA Standards of Nursing Practice
Assessment: The registered nurse collects comprehensive data pertinent to the patient’s health and/or the situation.
Diagnosis: The registered nurse analyses the assessment data to determine the diagnoses or issues.
Outcomes Identification: The registered nurse identifies expected outcomes for a plan individualized to the patient or the situation.
Planning: The registered nurse develops a plan that prescribes strategies and alternatives to attain expected outcomes.
Implementation: The registered nurse implements the identified plan.
Standards of Professional Performance
Professional performance standards ensure quality care and include ethical practice, ongoing education, evidence-based practice, leadership, and collaboration.
The ANA Code of Ethics guides nurses to deliver quality, ethical care, aligning with personal and professional values.
Professional Responsibilities and Roles
Nurses uphold roles requiring specific knowledge and skills, including:
Autonomy and Accountability: Independence in interventions and accountability for care quality.
Caregiver: Support for health, disease management, and functional independence.
Advocate: Protect patients’ rights and assist in asserting them.
Educator: Teach patients about health concepts, care routines, and self-management.
Communicator: Central to patient care, enabling coordination, emotional support, and clear information.
Manager: Coordinate care, manage resources, and support collaborative care environments.
Nursing: The profession focused on promoting health, preventing illness, and caring for patients with a holistic approach.
American Nurses Association (ANA): A professional organization that supports nurses with practice standards, advocacy, and resources to improve healthcare quality.
International Council of Nurses (ICN): A global organization that advocates for nursing standards and collaborative care across nations.
Caregiver: The nurse’s role in providing holistic care, including physical, emotional, social, and spiritual support to patients
Code of Ethics: Guidelines set by the ANA for nurses to provide ethical, quality care aligned with personal and professional values.
Registered Nurse (RN): A healthcare professional who has passed the NCLEX-RN® and is licensed to provide nursing care.
Educational programs available for professional registered nurse (RN) education.
The structure and content of professional education for registered nurses (RNs) in the United States has evolved to meet the increasing demand for competent, knowledgeable, and ethical nurses in a rapidly changing healthcare landscape The following are key aspects of RN education and its implications for professional practice.
Pathways to Becoming an RN
Associate Degree in Nursing (ADN): A two-year program typically offered by a community college, focusing on basic nursing skills and clinical experience. And there is the Bachelor of Science in Nursing (BSN): A four-year degree offered by universities, including a comprehensive curriculum in the social sciences, humanities, and critical thinking to support comprehensive nursing care. Both ADN and BSN students can sit for the NCLEX-RN® to become licensed RNs. However, there has been increasing emphasis on the BSN as an entry standard into the profession, especially with the recommendation of agencies such as the Institute of Medicine (IOM) that by 2020, 80% of RNs hold a BSN
Graduate and Advanced Nursing Education
Master’s Degree in Nursing (MSN): This bachelor’s degree prepares nurses for advanced roles such as nurse educators, administrators, nurse practitioners and advanced practice registered nurses (APRNs). Doctoral Degrees: Options include a Doctor of Nursing Practice (DNP) for clinical expertise and leadership, and a PhD, which is research-focused The American Association of Colleges of Nursing (AACN) recommends a DNP final degree for APRNs, emphasizing clinical application of research to improve patient outcomes.
Continuing and In-Service Education
Programs offered by universities, hospitals, and nursing organizations help nurses learn about new practices, technologies, and areas of expertise, and some states mandate continuing education to maintain licensure, while in-service education in healthcare organizations helps staff work on integrating new technologies and systems, and patients Practices to ensure competency and safe in care.
Standards of Practice and Nurse Practice Acts (NPAs)
The ANA establishes standards for the practice of nursing and a code of ethics to guide the practice of nursing. State NPAs define the legal process, ensure public safety and accountability. In recent years, NPA has expanded to include advanced practices for APRNs, such as prescribing authority and diagnostic authority.
Licensure and Certification
RNs in the US are required. all pass the NCLEX-RN® to establish basic knowledge and skills in states, while also becoming certified in specialties such as geriatric or critical care, progression that maintains this certification through education ongoing with the process of developing skills and performance.
Professional Nursing Organizations
Professional nursing organizations such as the ANA and specialty groups support nurses through professional development, policy advocacy, and professional standards. Student associations such as the National Student Nurses Association (NSNA) focus on preparing students for licensure and entry into the profession.
Advanced Practice Registered Nurse (APRN): A nurse with a master’s or doctoral degree who provides specialized care in roles like Nurse Practitioner, Clinical Nurse Specialist, Certified Nurse Midwife, and Certified Registered Nurse Anesthetist.
Continuing Education: Education that helps nurses stay updated on healthcare developments and maintain licensure.
In-Service Education: Training provided within healthcare institutions to update staff on new practices, policies, and technologies.
Nurse Educator: A nurse with specialized training in teaching who educates future nurses or patients in healthcare settings.
Nurse Practitioner (NP): An APRN who provides comprehensive care, often in primary care or specialized outpatient settings.
Roles and career opportunities for nurses
Nurses have numerous career paths, driven by healthcare innovations and expanding roles, including advanced practice roles and specialized care areas. They work directly with patients in settings ranging from hospitals to home care, focusing on health promotion and functional recovery.
Advanced Practice Registered Nurses (APRN)
Advanced practice registered nurse (APRN) roles encompass multiple specialties, each requiring advanced education and skills tailored to specific populations, such as paediatrics, adult-geriatrics, and mental health. These roles include Clinical Nurse Specialists (CNS), who are experts in specialized fields like geriatrics or diabetes care; Certified Nurse Practitioners (CNP), who provide primary and specialty care; Certified Nurse Midwives (CNM), focusing on women’s health and childbirth; and Certified Registered Nurse Anesthetists (CRNA), who specialize in administering anaesthesia.
Advanced Practice Roles in Professional Nursing
Advanced practice roles in nursing include Nurse Practitioners (NPs), who provide holistic healthcare by managing patient health, particularly for those with chronic conditions, often in outpatient and community-based settings, forming collaborative, ongoing relationships with patients to address a broad range of health needs. Certified Nurse-Midwives (CNMs) specialize in midwifery, offering care for women during pregnancy, labor, delivery, the postpartum period, and general gynecological services, focusing on natural childbirth and primary reproductive health care while operating independently. Certified Registered Nurse Anesthetists (CRNAs) deliver anesthesia services, requiring advanced education in anesthesia and at least a year of critical care experience, working closely with anesthesiologists to ensure patient safety throughout anesthesia care. Clinical Nurse Specialists (CNS) are experts in specific areas, such as geriatrics or diabetes, providing advanced care, consulting, and support to both patients and staff.
Educational and Administrative Professional Nursing Roles
Educational and administrative nursing roles encompass a range of responsibilities aimed at advancing nursing practice, education, and healthcare delivery. Nurse Educators play a vital role in preparing future nurses, often working in academic or hospital-based settings, and may also focus on patient education in specialized areas such as wound care or diabetes management. They require both practical and theoretical expertise, frequently supported by advanced degrees. Nurse Administrators manage patient care delivery within healthcare organizations, handling tasks such as budgeting, staffing, program planning, and personnel development, with higher-level administrators overseeing multiple units and often holding advanced degrees in nursing or business. Nurse Researchers focus on conducting research to enhance patient outcomes and advance nursing practices, typically working in academic, hospital, or independent settings and holding advanced degrees, such as a doctorate or a master’s degree.
Challenges in Professional Nursing: Addressing the Nursing Shortage
The nursing profession faces significant challenges from a severe shortage of registered nurses, which affects patient care, employment, and education, and makes attracting and retaining skilled workers important Studies highlight the importance of provide RN care that will provide better patient quality, fewer complications, and faster recovery with , where It emphasizes the need for educated, conservative recruitment strategies who has been emphasized to high standards of nursing practice. Nurses must adopt effective time management, medical communication, and patient education strategies to reduce stress caused by resource scarcity. It also ensures nurses are retained, even in dire circumstances.
Certified Nurse-Midwife (CNM): An APRN who specializes in women’s health, providing care through pregnancy, childbirth, and postpartum.
Certified Registered Nurse Anaesthetist (CRNA): An APRN with expertise in anaesthesia, responsible for providing anaesthesia care across various settings.
Clinical Nurse Specialist (CNS): An APRN specializing in specific areas (e.g., geriatrics, diabetes) to offer expert patient care and consultation.
Nurse Administrator: A nurse who oversees operations in healthcare settings, including budgeting, staffing, and patient care delivery.
Nurse Researcher: A nurse focused on conducting studies to improve healthcare outcomes and nursing practices.
Influence of social, historical, political, and economic changes on nursing practices
Historical influences on Professionalism in Nursing
Nurses respond to the needs of the community over time. For example during wars, health crises, and community health challenges such as disease outbreaks. Programs such as advocacy campaigns and health education have been implemented to help vulnerable populations. Florence Nightingale greatly influenced nursing with her philosophy of health care and restoration. During the Crimean War, she pioneered epidemiology by using statistical analysis to link poor sanitation to high mortality rates, resulting in a significant reduction in mortality as well as establishing a nursing training program that was formerly organized at St Thomas’ Hospital in London.
Nursing made great strides in the United States during the Civil War. Prominent figures such as Clara Barton, founder of the American Red Cross, and Mother Bickerdyke, who organized ambulance service, helped check war. Harriet Tubman actively supported soldiers on the Underground Railroad, the first professionally trained African-American nurse Mary Mahoney championed multiculturalism in health care Community nursing also expanded during this time, while Lillian Wald and Mary Brewster founded the Henry Street Residence in New York which aims to meet the health needs of impoverished communities.
In the twentieth century, nursing roles became increasingly specialized. Nurse-midwifery emerged as a profession, and advanced nursing education programs grew. Education milestones included Mary Adelaide Nutting’s efforts to integrate nursing into university curricula, making her the first nursing professor at Columbia Teacher’s College. The establishment of the Army and Navy Nurse Corps and specialty programs further enhanced the profession.
By the twenty-first century, nursing practices adapted to modern challenges, such as an aging population, bioterrorism, emerging infections, and disaster management. Updated curricula now emphasize the integration of technology and informatics to ensure efficient, high-quality patient care, meeting the evolving needs of the healthcare landscape.
Political and Policy Influence on Professional Nursing
Nurses are becoming more active in health policy, advocating for legislation that supports patient care improvements and public health initiatives. Professional organizations like the American Nurses Association (ANA) work to raise healthcare standards and ensure access to high-quality care. Moreover, nurses lobby for programs such as home visits for high-risk mothers, which help reduce newborn mortality and improve overall health outcomes in underserved communities.
Current trends in nursing
The nursing profession continues to adapt to the changing health care landscape, which is shaped by technological advances, changing patient needs, and changing societal expectations
Evidence-based practice (EBP) ensures that clinical decisions are guided by up-to-date research data rather than tradition or past experience. This approach enhances patient safety and quality of care, while demonstrating organizational accountability to stakeholders. Nurses are increasingly involved in the use of scientific data for treatment planning, relying on up-to-date journals and established methodologies for informed clinical practice.
The Quality and Safety Education for Nurses (QSEN) program prepares nurses with skills in patient-centered care, teamwork, evidence-based practice, quality improvement, safety, and advocacy. It focuses on essential knowledge, skills, and attitudes (KSAs). increase access to high quality care. Nurses are trained to involve patients and families in care decisions, use data to continuously improve quality, and prioritize safety through improved communication and collaboration.
More Trends in Professional Nursing
Advances in telehealth records, electronic health records (EHRs), and decision support systems are changing how patient care is delivered. These tools improve research, support evidence-based practice, and improve communication across health care settings. Nurses need to master these technologies to improve data management, mobility, and informed clinical decision making. In addition, integrating genomic data into patient care requires nurses to have knowledge of genetics and its use.
Genomics enables self-care by providing insight into patients’ genetic characteristics in some cases. Nurses play an important role in family history screening, educating patients about genetic risk factors, and promoting preventive measures. For example, patients with a family history of a particular cancer are directed to early screening and interventions with genomic data.
Nurses are recognized as important frontline healthcare professionals. Accessible data, such as the Hospital Consumer Assessment of Healthcare Provider Systems (HCAHPS) influence public opinion by providing information about hospital quality and safety. Nurses are encouraged to remain active, as the quality of their care directly affects public trust and the reputation of healthcare organizations.
Professional Nursing issues
Nurses’ own care and compassion fatigue:
Prolonged involvement in patients’ suffering can lead to compassion fatigue, emotional exhaustion, burnout, and dysfunction. Wellness programs that focus on resilience and stress management are essential to prevent burnout and support a healthy nursing workforce. These programs contribute to nurses’ well-being, improve job satisfaction, and improve patient care.
The Affordable Care Act (ACA) and rising health care costs:
The ACA emphasizes health promotion, disease prevention, and community-based care, where nurses must adapt their practices to these goals. Rising health care costs require nurses to provide high-quality care in a cost-effective way, using resources efficiently to optimize patient outcomes while supporting organizations’ financial stability.
Demographic shifts
An older population is seeking expanded access to health care, particularly in inpatient, community, and home care. Increasing urbanization and chronic diseases require transformative health care systems and resources to better meet these changing demographic needs.
Medically Underserved Populations
Unemployment, low-income jobs, mental health challenges, and homelessness contribute to the rising demand for healthcare services among underserved populations. The increasing costs of home-based and palliative care further restrict access, leading many patients to forgo essential care due to financial constraints. Addressing these barriers is critical to ensuring equitable and comprehensive healthcare delivery.
Genomics: The study of genes and their effects on health, enabling nurses to provide personalized care based on genetic predispositions.
Patient Advocate: The role of a nurse in supporting and protecting patients’ rights within healthcare.
Professional Organization: Groups like the ANA that support nursing professionals with resources, standards, and advocacy efforts.
Quality and Safety Education for Nurses (QSEN): An initiative aimed at equipping nurses with competencies in quality care, safety, teamwork, and patient-centered practices.
