The Healthcare System
This chapter will give an understanding of the structure of the United States healthcare system. This is including public and private resources. It will explore the different ways in which healthcare is funded, such as insurance models and government programs, and will see different places where healthcare is delivered.
By the end of this section, you should be able to know about the:
- Structure of the United States health system.
- Various methods for financing health care.
- Types of settings that provide various health care services.
Let’s take a closer look at them.
Test Your Knowledge
At the end of this section, take a fast and free pop quiz to see how much you know about The Health Care Delivery System.
Structure of the US healthcare system
The U.S. healthcare system is complex, with a wide range of services from various health professionals. However, access to care can be difficult, particularly for uninsured individuals who often delay or skip treatment. this will increase health risks. Rising costs from technological advancements and new medications have led health care to operate more as a business than a service. posing challenges such as reducing costs, improving access, and promoting healthy behaviors. Discharge practices have shifted, with earlier discharges requiring more patients to rely on home care or nursing homes, often with family support. Nurses play a key role in ensuring continuity of care across settings.
The U.S. healthcare system also includes specialized services in a variety of areas, from health promotion to restorative care. Nurse-run clinics emphasize health promotion, education, chronic disease management, and caregiver support. They are providing services such as health risk assessment, wellness counseling, supervision intensive and long-term provision for Block and Parish Nurses living in communities providing services to older adults or homebound individuals of nursing participate, helping to fill gaps not addressed by traditional health care. These services include transportation, transportation, recreational services, domestic worker support, and spiritual healthcare system support. Community health centers are outpatient clinics focused on the primary care of specific populations, usually affiliated with hospitals or community organizations. Those centers provide physical examinations, health screenings, diseases services, education, and counseling.
Nursing and Healthcare System Values
Nursing is a discipline that focuses on caring and compassion, focused on helping people regain or maintain health and find comfort. Modern healthcare system, driven by cost-saving strategies. This often creates tension between care and professional priorities. The Institute of Medicine (IOM) calls for safe, effective, patient-centered and equitable delivery systems (IOM, 2001). The National Priority Partnership, a group of 52 health organizations, aims to transform health care by focusing on healthy communities and by prioritizing affordable care teeth.
Promote good practice in health and wellbeing.
Effective prevention and intervention of major diseases.
To ensure patient-centered, safe and affordable care.
Vision for Healthcare System Transformation
IOM ensures access to healthcare for all, emphasizing wellness, prevention and compassionate care. This shift challenges nursing to maintain its patient-centered values and adapt to changing roles, and requires nurses to:
Take full advantage of your training.
Get a higher education for career advancement.
Partnerships with other healthcare providers in new healthcare system settings.
Increase the use of data and information for executive planning.
Healthcare System Regulation and Reform
Historically, there was no incentive to control costs, and new payers paid more for care. Rising costs have led to regulatory changes. Such as the emergence of Professional Standards Review Organizations (PSROs) and Physician-Review Utilization (UR) committees to review Medicare-related clinical care.
The Prospective Payment System (PPS), established by Congress in 1983, shifted Medicare reimbursements to a diagnosis-related group (DRG) model with fixed payments. Capitation, a payment model where providers receive a set fee per patient, incentivizes efficient care and has influenced practices across health care settings, resulting in shorter hospital stays and increased demand for home healthcare system.
Medicare: A federal health insurance program primarily for people. Those people aged 65 and older or with certain disabilities, covering hospital and medical costs.
Key Drivers of Change in Health Care System
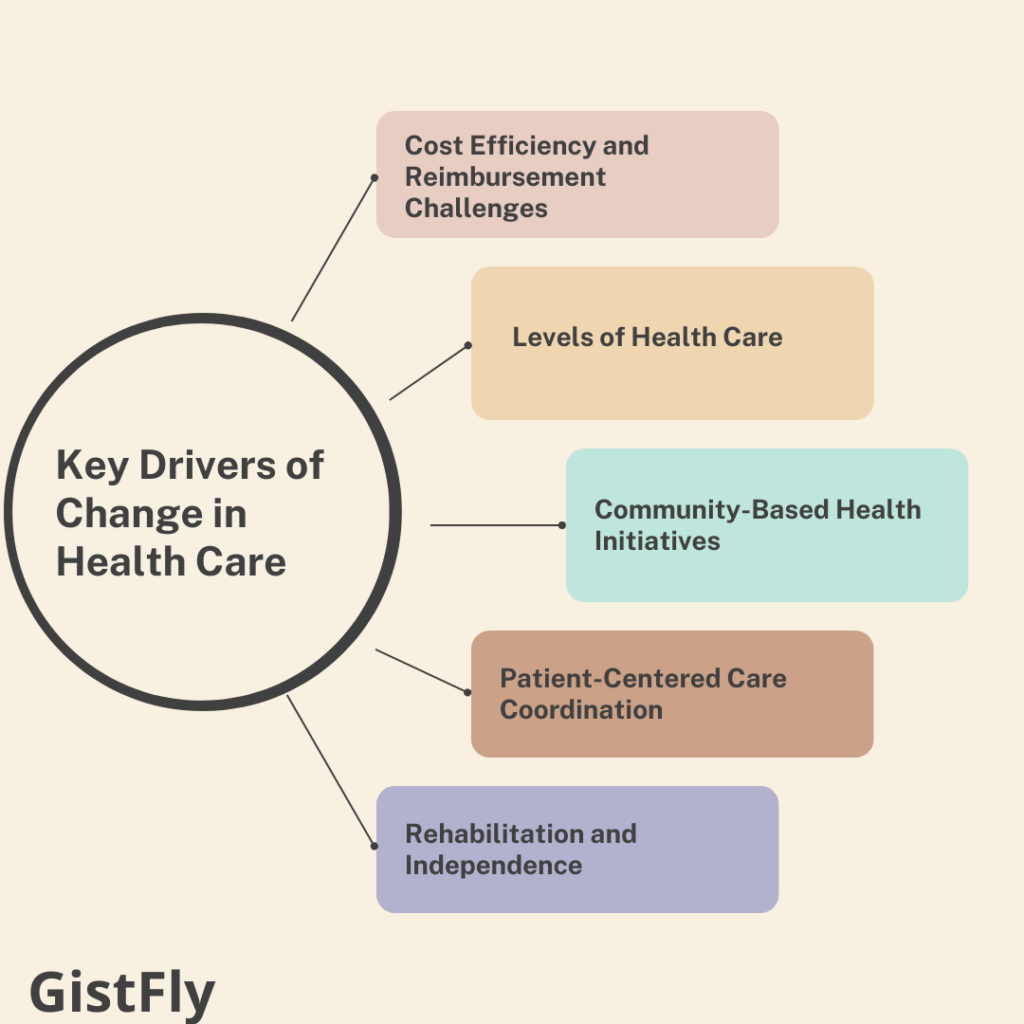
Cost Efficiency and Reimbursement Challenges of health care system
Rising healthcare costs and decreasing reimbursement rates compel institutions to find ways to deliver care more efficiently while maintaining quality. The Medicare prospective reimbursement system calculates payments based on Diagnosis-Related Groups (DRGs). Which incentivizes hospitals to manage resources effectively.
Levels of healthcare system
Health care encompasses a range of services and settings tailored to patients at various stages of health and illness. Effective health promotion strategies occur across home, workplace, and community settings, emphasizing preventive care and wellness.
Community-Based Health Care Initiatives
Nurses play a critical role in promoting health within communities, tackling the challenge of maintaining population health outside of traditional clinical settings. Successful community health programs are built on strong relationships with community members, respecting and integrating cultural and environmental factors into healthcare system plans.
Patient-Centered Health Care Coordination
Hospitalized patients often present acute health issues. Which necessitate careful coordination of care, especially prior to discharge. Discharge planning is initiated upon admission, facilitating smooth transitions for patients moving from one healthcare environment to another.
Rehabilitation and Independence of Healthcare System
The rehabilitation goal is to help individuals regain normal or near-normal function. This is after experiencing physical or mental health challenges. Home care agencies play a vital role in providing diverse services. Those agencies prioritize patient and family independence, reflecting a shift towards care in the home setting.
Health care organizations are increasingly evaluated based on a range of outcomes, including:
Prevention of complications: Implementing preventive measures to reduce adverse health events. Functional outcomes for patients: Assessing how well patients can perform daily activities post-treatment. Patient satisfaction: Gathering feedback to enhance care experiences.
Nurses must stay informed and proactive about health care delivery system issues to provide high-quality care and positively influence health outcomes.
Importance of Quality Improvement and Patient Engagement
Continuous analysis of quality improvement (QI) data allows clinicians to understand work processes and identify areas that need practice changes. Engaging patients and families in care decisions is crucial for satisfaction and positive health outcomes. Also underscoring the shift toward patient- and family-centered care.
Capitation: A payment model in healthcare where providers are paid a fixed amount per patient regardless of the number of services provided, promoting cost-effective care.
Diagnosis-Related Groups (DRGs): A system categorizing hospitalization costs to standardize Medicare reimbursements, based on diagnosis and treatment.
Patient-Centered Care: A healthcare system approach that respects and responds to patient preferences, needs, and values in all care decisions.
Rehabilitation: Therapeutic services aimed at restoring patients’ physical, mental, and social abilities after illness or injury.
Various Methods for Financing Health Care System
Managed care programs, which receive fixed per-patient payments, emphasize disease prevention, early intervention, and outpatient care to reduce costs and promote health effects. This develop a variety of insurance policies within this framework, including managed care organizations (MCOs). For non-network care Medicare, the primary government program for individuals age 65 and older, including hospital (Part A), medical (Part B). Managed care (Part C), and drugs prescription (Part D) includes Medicaid, a joint federal and state program that provides health coverage for low-income individuals, including children, pregnant women and the elderly; private insurance. This operates on a pay-for-performance basis with significant out-of-pocket expenses; long-term care (LTC) insurance. which covers extended care; and the National Children’s Health Insurance Program (SCHIP), which provides health coverage for uninsured children who do not qualify for Medicaid. In terms of quality control and safety.
Other Methods
The National Quality Forum (Never Events” identifies serious and preventable events that should be reported and merit Medicare reimbursement for these errors. Moreover, motivates healthcare system organizations to provide options prevention (PPACA) also aims to expand access, reduce costs and improve care-quality. Key provisions of the PPACA include mandated health insurance for all individuals or tax penalties. Those expanded eligibility for Medicaid and state children’s insurance programs, creation of health insurance exchanges, prohibition of insurers from denying coverage based on health status or gender, penalties for large employers not offering health coverage, and allowing adult children up to age 26 to remain on their parents’ insurance plans.
Medicaid: A federal and state program offering healthcare system coverage for low-income individuals, families, and specific vulnerable populations.
Types of settings that provide various health care services.
The U.S. health system provides services at five major levels: disease prevention, health promotion, primary, secondary, and secondary care and these services are delivered in a variety of areas, including disease prevention, primary, secondary, tertiary, recycling, and ongoing environment. Many large health systems use integrated delivery networks (IDNs) to streamline services at these levels. reducing redundancies and ensuring patients receive care in the most appropriate setting.
Primary care focused on health promotion includes services such as prenatal and wellness care for babies, nutritional counseling, wellness programs such as family planning, yoga and meditation. Preventive care aims of the mouth include blood pressure and cancer screening, vaccinations, mental health support, community safety regulations (e.g. seat belts and anti-texting laws). Diseases are prevented through activities such as secondary acute care provides emergency services for acute conditions, complex medical and surgical procedures, and radiology (such as X-rays and CT scans). The tertiary level of care some specialized acute services, including intensive care units (ICUs) and sub-acute. There are also care facilities. Restorative care supports rehabilitation and rehabilitation, providing services such as cardiac orthopedic rehabilitation, spinal cord injury programs, and home care. Continuing care primarily consists of long-term support such as assisted living and mental health day care for the elderly or chronically ill.
Other Types of Settings
The health reform has shifted the focus to wellness and preventive care by devoting more resources to specialized preventive services. These changes emphasize the importance of nurses as patient advocates, contributing to continuity in care rates and improved health outcomes. Nurses also play a critical role in effectively meeting patient needs across all levels of care and providing leadership in communities and health systems.
Accreditation and certification are critical for healthcare system organizations to demonstrate their commitment to quality and safety. Accreditation applies to all organizations, while certification focuses on specific programs or projects. Agencies such as The Joint Commission (TJC) provide accreditation in a variety of care settings, including hospital, long-term care, and behavioral health care. Specialized organizations such as the Commission on Accreditation of Rehabilitation Facilities (CARF) and Community Health Accreditation Program (CHAP) focus on specific areas of care.
Primary health policy
Primary health policy focuses on improving population health outcomes through services such as education, nutrition, maternal/child health, family planning, immunization, and disease prevention. Equity, trust, and improving accountability in health care delivery requires collaboration among health professionals, community leaders, and members. Health promotion programs are primary centers of patient care. This reducing healthcare system costs by reducing the incidence of disease and the need for expensive treatments.
Examples of primary healthcare system preventive services include school health programs, which integrate health promotion into the school curriculum of life skills, nutrition, physical activity, health screening, crisis intervention etc. and safety through employment a promoting and reducing absenteeism through services such as disease prevention. Physicians’ offices routinely provide primary care and health screening, including nurses who the practice often collaborates with physicians to manage chronic conditions such as diabetes and arthritis.
Secondary and tertiary care primarily involve diagnosing and treating illnesses that require more complex and costly interventions. Secondary care is provided in settings like emergency rooms, urgent care centers, and inpatient units for acute health issues. Tertiary care includes intensive care units (ICUs) for the most critical conditions. The Patient Protection and Affordable Care Act (PPACA) has expanded insurance coverage for young adults. This is reducing the likelihood of delaying care due to lack of insurance. Additionally, many procedures that previously required hospitalization, such as certain surgeries, are now done in outpatient settings, helping to reduce costs.
Access to Health Care System
Hospitals provide comprehensive secondary and tertiary care services, from emergency and critical care to specialized inpatient services. Discharge planning is essential and begins upon admission to ensure continuity of care. This is involving coordinated efforts from an interdisciplinary healthcare system team, education on medication administration and rehabilitation techniques, and referrals to community resources. Intensive Care Units (ICUs) offer intensive monitoring and care for life-threatening conditions, utilizing advanced technologies like ventilators and cardiac monitors, and are highly resource-intensive due to specialized care needs. Psychiatric facilities offer specialized care for emotional and behavioral health issues, such as depression and eating disorders, through both inpatient and outpatient services, with an interdisciplinary team developing comprehensive care plans to support patients’ return to functional life in the community.
Access to health care in rural areas can be difficult. Many rural hospitals now operate as community-based critical care facilities (CAHs), providing essential services such as 24-hour emergency care for critically ill patients, providing basic assessment to those seeking admission to large remote areas medical and large health systems Access to specialist counseling in rural hospitals due to affiliation has been improved, improving the quality of care.
Restorative healthcare system helps patients recover from illness or disability and regain independence. With short hospital stays. Many patients continue to recover in a rehab facility. Key components of rehabilitative care include physical rehabilitation (such as wound care and exercise interventions) and education for patients and families to ensure understanding of recovery goals, risks feasibility, and the need to follow a treatment plan.
Acute Care definition: Short-term treatment for patients with severe or urgent medical conditions, typically provided in hospitals or specialized facilities.
Adult Day Care Centers: Facilities offering social and health services during the day for older adults or individuals with disabilities who need supervision.
Assisted Living: Residential settings providing personal care support, including assistance with daily activities, while allowing residents to maintain a level of independence.
Discharge Planning: The process of preparing a patient to leave a healthcare system facility and arranging necessary follow-up care for a smooth transition.
